SMALL WONDER: Complex EGFR mutation showing exquisite response to Afatinib
SMALL WONDER: Complex EGFR mutation showing exquisite response to Afatinib
Shaunak Valame*, Dr Dhruti Manek1
1. Department of Pathology, Jawaharlal Nehru Cancer hospital, Bhopal.
*Correspondence to: Shaunak Valame, Department of Oncology, Bhopal, India.
Copyright.
© 2024 Shaunak Valame. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 04 July 2024
Published: 01 August 2024
Abstract
Small molecule Tyrosine Kinase Inhibitors have revolutionised the treatment landscape of driver mutation positive Non-Small Cell Lung Cancer. Complex EGFR mutations - two different EGFR mutations within the same tumour, are found in approximately 3-7% of patients. This case report describes the treatment effect of Afatinib on a patient who presented with complex EGFR mutations in exon 18 – Gly719Ala (G719A) and Glu709Ala (E709A). The report adds to the growing literature on options to tackle complex EGFR mutations.
KEYWORDS (MeSH): Carcinoma, Non-Small-Cell Lung; Epidermal Growth Factor; Tyrosine Protein Kinase Inhibitors; Afatinib
SMALL WONDER: Complex EGFR mutation showing exquisite response to Afatinib
Introduction
Small molecule Tyrosine Kinase Inhibitors (TKI) have revolutionised the treatment landscape of driver mutation positive Non-Small Cell Lung Cancer (NSCLC). Activating mutations in the EGFR gene occur in more than 50% of Asian patient with advanced NSCLC1. The classical EGFR mutations (exon 19 deletions and L858R substitution in exon 21) account for approximately 85% of sensitising mutations2. Uncommon mutations accounting for the remaining 15% are point mutations or duplications in exons 18 - 21, de novo T790M mutations in exon 20, or exon 20 insertions3. Complex EGFR mutations, which are two different EGFR mutations within the same tumour, are rarer still – found in approximately 3-7% of patients4. As clinical trials have excluded patients harboring such uncommon mutations, outcomes of therapy have not been fully elucidated. Here we present a case of NSCLC with complex EGFR mutation and its response to therapy.
Case History
A 67-year-old non-smoking female presented in October 2021 with a 3-month history of cough with expectoration, loss of appetite, and significant weight loss. Her Eastern Cooperative Oncology Group Performance Status (ECOG PS) was 2. She had done a CT scan at a different centre in September 2021 which showed an 87x71x49mm right lung lower lobe lesion, mediastinal lymphadenopathy, and liver lesions. Biopsy done from the lung lesion revealed Adenocarcinoma which was confirmed to be of pulmonary origin through immunohistochemistry which showed TTF1 and Napsin A positivity. Staging PET-CT (Fig 1A & 1B) revealed metabolically active right lower lobe lung lesion, hypermetabolic metastatic mediastinal & retroperitoneal lymphadenopathy (largest coeliac lymph node), active peritoneal soft tissue deposit in right paracolic region and multiple bilobar hepatic metastatic lesions. Contrast MRI brain showed no evidence of disease. Molecular Lung Panel by Next Generation Sequencing detected 2 missense mutations in EGFR exon 18 – Gly719Ala (G719A) and Glu709Ala (E709A). She was started on Afatinib 30 mg/d on 27th October 2021. After 1 month of therapy, she developed grade 2 diarrhoea as per CTCAE and was managed conservatively. By this time, her cough had resolved. Dose increment to 40 mg was discussed with the patient but she opted to continue the same dosage. After completing 3 months of therapy, her ECOG PS had improved to 0. She had grade 1 diarrhoea and grade 2 dysgeusia as per CTCAE. Response evaluation PET CT (Fig 1C & 1D) scan on 27th January 2022 showed significant metabolic response and volume reduction in lung lesion, mediastinal and retroperitoneal lymphadenopathy, peritoneal deposit and also in bilobar hepatic lesions (Table 1). She took Afatinib therapy at 30mg/d till April 2022 before being lost to follow-up.
|
TABLE 1. Target Lesion |
Staging PET CT October 2021 |
Response Evaluation PET CT January 2022 |
||
|
Size (mm) |
SUV max (gm/ml) |
Size (mm) |
SUV max (gm/ml) |
|
|
Right Lung Lower Lobe |
46x60x60 |
11.86 |
23x33 |
3.16 |
|
Mediastinal LN (largest) |
25x21 |
11.38 |
9x8 |
4.46 |
|
Retroperitoneal LN (largest) |
24x21x20 |
10.8 |
13 |
10.32 |
|
Liver (largest in segment III) |
43x57x41 |
14.65 |
23x27 |
4.52 |
|
Peritoneal deposit |
19x18 |
5.8 |
8 |
5.52 |
Discussion
With Oncologists opting for comprehensive genomic profiling in advanced NSCLC, uncommon and complex EGFR mutations are being revealed. Due to their low prevalence and sparse data on treatment options, they are challenging to treat.
The largest study5 to analyse treatment outcomes in EGFR exon 18 mutated NSCLC found that the most common exon 18 mutations were G719X (75.6%) followed by E709X (15.9%). The most common subtype of G719X mutation was G719A (53.6%). Complex mutations involving G719X were observed in 41.5% patient in their study. However, they did not come across the complex mutation combination of G719A + E709A as seen in our patient.
Most of the landmark EGFR TKI trials exclude the subset of patients with non-canonical and complex mutations. However, the LUX-Lung trials did permit enrollment. A post-hoc pooled analysis of the LUX-Lung trials3 observed an Objective Response Rate (ORR) of 71.1%, median Progression Free Survival (PFS) of 10.7 months, and median Overall Survival (OS) of 19.4 months in patient with point mutations or duplications in exon 18 – 21.
Complex mutations present a different challenge in selecting the best TKI. Wu et al6 found that in comparison with common EGFR mutations, patients with rare and complex mutations, had a significantly worse ORR (74.1% vs 47.5%, respectively), and a poorer PFS (8.5 months vs 5.0 months). In their series, mutations of E709X did not exist alone, but were all complex mutations occurring with G719X or L858R. The single patient who had complex mutation involving E709G + G719C showed disease progression.
An in vitro study showed G719A, E709K, and del18 mutations having high sensitivity to Afatinib or Neratinib when compared to 1st and 3rd generation EGFR TKI.7 Moreover, ORR in G719X single mutation tumours was 32%, while higher ORR was observed for E709X (53%) and G719X (59%) complex mutations. Partial response to Afatinib was seen in E709X + G719X after treatment with 1st generation TKI8. In a seminal study, Kobayashi et al9 discussed how not all EGFR mutations are created equal. Mutation specific TKI selection may help in maximizing benefit for those harboring less sensitive mutations.
The protagonist of this case study, with a complex E709A + G719A EGFR Exon 18 mutation, has shown a near complete response to 3 months of Afatinib therapy. Although one swallow does not make a summer, this case adds clinical experience to responses shown in complex EGFR mutations. It also widens the repertoire of mutations targetable by Afatinib.
IMAGE 1
1A) Right Lung lower lobe mass (pre-treatment)
1B) Metastatic Liver lesions (pre-treatment)
1C) Right Lung lower lobe mass showing significant metabolic response after 3 months of Afatinib
1D) Liver lesions showing significant metabolic response after 3 months of Afatinib
References
1. Y. Shi, et al.; A prospective, molecular epidemiology study of EGFR mutations in asian patients with advanced non–small-cell lung cancer of adenocarcinoma histology (PIONEER); J. Thorac. Oncol. 9 (2) (2014) 154–162.
2. T.J. Lynch, et al., Activating mutations in the epidermal growth factor receptor underlying responsiveness of non–small-cell lung cancer to gefitinib, N. Engl. J. Med. 350 (21) (2004) 2129–2139.
3. Yang JC, Sequist LV, Geater SL, Tsai CM, Mok TS, Schuler M, et al. Clinical Activity of Afatinib in Patients With Advanced Non-Small-Cell Lung Cancer Harbouring Uncommon EGFR Mutations: A Combined Post-Hoc Analysis of LUX-Lung2, LUX-Lung-3, and LUX-Lung6. Lancet Oncol (2015) 16 (7):830–8.
4. Hata A, Yoshioka, H, Fujita S et al. Complex mutations in the epidermal growth factor receptor gene in non-small cell lung cancer. J Thorac Oncol; 2010; 5:1524-1528
5. Xu H, Yang G, Li W, Li J, Hao X, Xing P, Yang Y and Wang Y (2021) EGFR Exon 18 Mutations in Advanced Non-Small Cell Lung Cancer: A Real-World Study on Diverse Treatment Patterns and Clinical Outcomes. Front. Oncol. 11:713483.
6. Wu JY, Yu CJ, Chang YC, Yang CH, Shih JY, Yang PC. Effectiveness of tyrosine kinase inhibitors on “uncommon” epidermal growth factor receptor mutations of unknown clinical significance in non-small cell lung cancer. Clin Cancer Res 2011; 17:3812–3821.
7. Kobayashi Y, Togashi Y, Yatabe Y, et al. EGFR exon 18 mutations in lung cancer: molecular predictors of augmented sensitivity to afatinib and neratinib as compared with first or third generation TKIs. Clin Cancer Res 2015; 21: 5305 – 13.
8. Heigener DF, Schumann C, Sebastian M et al. Afatinib in non-small cell lung cancer harboring uncommon EGFR mutations pretreated with reversible EGFR inhibitors. Oncologist 2015; 20: 1167 – 74.
9. Y. Kobayashi, T. Mitsudomi, Not all epidermal growth factor receptor mutations in lung cancer are created equal: perspectives for individualized treatment strategy, Cancer Sci. 107 (2016) 1179–1186.
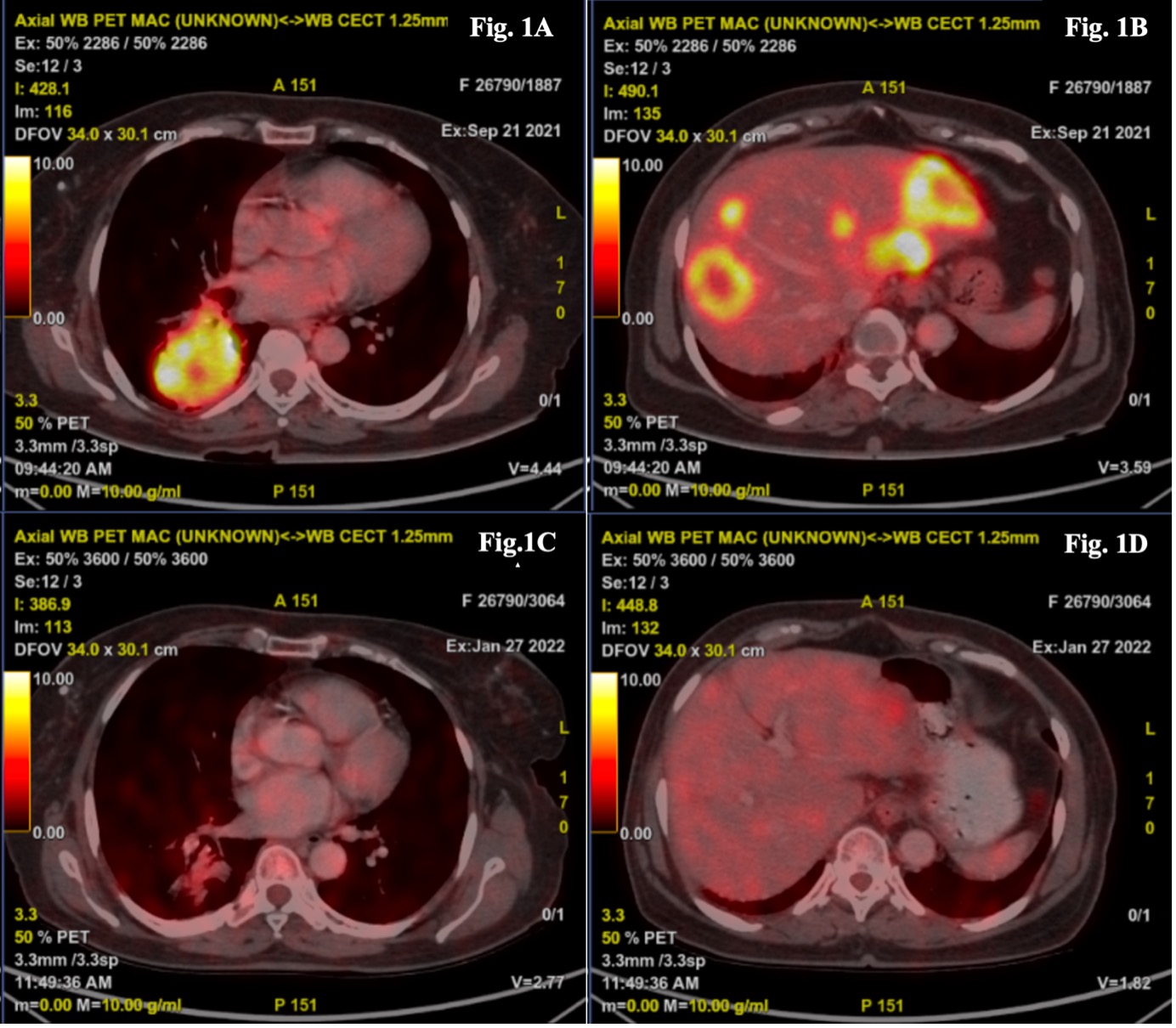
Figure 1
