Factors Associated with Delayed Presentation of Breast Cancer among Nepali Women
Factors Associated with Delayed Presentation of Breast Cancer among Nepali Women
Arun Shahi1*, Amul Shrestha2, Venkata Pradeep Babu Koyola3, Bibhuti Shahi4, Gill Morgan5
1. Arun Shahi, MD, MPH, Assistant Professor of Medical Oncology, Patan Academy of Health Sciences, Nepal
2. Amul Shrestha, MPH, Program Coordinator, Innovative Foundation for Health and Research, Nepal.
3. Venkata Pradeep Babu Koyyla MD, DNB, Director, Medical Oncology, Shankara Cancer and Research Institute, Tezpur, Assam 784154.
4. Bibhuti Shahi MD, Consultant, Gynecology and Obstetrics, Sukhi Pariwaar Clinic, Kathmandu, Nepal.
5. Gill Morgan MD Director Oncoalert.
*Correspondence to: Arun Shahi, MD, MPH, Assistant Professor of Medical Oncology, Patan Academy of Health Sciences, Nepal.
Copyright.
© 2024 Arun Shahi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 10 July 2024
Published: 01 Aug 2024
DOI: https://doi.org/10.5281/zenodo.13948782
Abstract
Background: Breast Cancer is the leading cause of cancer mortality among women in Nepal. Delayed presentation is preventable and has major effects on a patient's prognosis and survival. This study aimed to identify the extent of delayed presentation and its associated factors in women with breast cancer in Nepal.
Methods: This cross-sectional study was conducted from Jan 2020 to December 2023 at Patan Academy of Health Sciences (PAHS), HAMS and B&B hospital. Respondents had histologically confirmed breast cancer. All Breast Cancer patients admitted into the department of medical oncology of PAHS were selected by purposive sampling technique. Face to Face interviews were conducted using standardized questionnaires. We measured the time from the first recognition of symptoms to the first physician’s consultation and to the histological diagnosis of breast cancer. Diagnosis delay was defined when there was more than 6 months’ delay from the recognition of symptoms to the histological diagnosis. Multiple logistic regression was used for analysis.
Results: Two hundred and forty-six (246) patients met the inclusion criteria. The mean age was 44 years. Most respondents were married housewives with a median family income of US $ 100 per month. The median time to consultation was 2.9 months and the median time to diagnosis was 7.5 months. The frequency of diagnosis delay of more than 3 months was 86.4% and delay of more than 6 months occurred in 65.5% of the cases. The factors associated with diagnosis delay included the use of alternative therapy (homeopathy), feeling of hesitation, breast ulcer, non-cancer interpretation, negative attitude toward treatment, and negative family history of breast cancer.
Conclusions: A significant percentage of women with breast cancer in Nepal are experiencing presentation delay. Delays in consultation and diagnosis are serious problems in Nepal. Coordinated efforts on Breast cancer awareness and education are required to promote early detection, diagnosis and treatment before the tumors enlarge and metastasis.
Key Words: Breast cancer, delay in presentation, menopause, hormone receptors, presentation time, stages of breast cancer (I, II, III, IV).
Factors Associated with Delayed Presentation of Breast Cancer among Nepali Women
Introduction
Breast cancer is the most common and deadliest cancer in women worldwide (1,2). In high-resource countries, the incidence and mortality rates of breast cancer have been declining, whereas in low-resource countries, the incidence and mortality rates have been increasing because of the differences in the access to breast cancer early detection (2). Every year about 522,000 women die due to breast cancer worldwide and has become a dominant cause of death rate in women (3). Breast cancer is known to occur when cells in the breast go out of control and the most common of all cancers is invasive ductal carcinoma however other common kinds include Paget’s disease, external icon medullary, mucinous, and inflammatory breast cancer (3). It has become a growing social problem in many communities as the global incidence has increased to about 12.5% (i.e. one out of 8 women) suffer from it (4).
Breast cancer is a substantial social and economic burden in Nepal. Prevention has been demonstrated to be among the most effective long-term strategies to lessen the increasing chronic disease burden (5). However, due to socioeconomic disparities and insufficient financial resources, to date, the prevention of breast cancer has not been well conducted in Nepal (6). Delay in seeking examinations of breast symptoms is a significant problem associated with a lower breast cancer survival rate (5, 6).
As a developing nation, Nepal is faced with several challenges with regards to the care of patients with breast cancer with inadequate funding; the uneven distribution of resources and services; inadequate numbers, training and distribution of health-care personnel and equipment; and a lack of adequate care for many populations based on socioeconomic and geographic factors (7).
It is important to provide awareness to communities that any breast symptoms should prompt early medical attention because they potentially could indicate breast cancer. The study aim was to investigate the potential factors associated with delay in seeking treatment among patients with breast cancer at PAHS (Patan Academy of Health Sciences), HAMS (Hospital for Advanced Medicine and Surgery) and B&B (Baidya and Banskota) hospital of Kathmandu and Lalitpur districts of Nepal.
Methods
A cross-sectional study was conducted at three different hospitals in Kathmandu valley, viz. Patan Academy of Health Sciences, HAMS and B&B from January 2020 to December 2023. Purposive Sampling technique was applied for the data collection purpose where the study participants were "all the HPR diagnosed female breast cancer patients, age 30-70 years". Face-to-face interview was conducted using a standardized questionnaire.
We measured the time from the first recognition of symptoms to the first physician’s consultation and to the histological diagnosis of breast cancer. Diagnosis delay was defined when there was more than 6 months’ delay from the recognition of symptoms to the histological diagnosis. A total of 246 cases were surveyed and the responses containing anonymized data were collected and analyzed using SPSS-version-20. The results were interpreted and were checked with various socio-demographic and clinical factors using the chi-square test and multiple logistic regression model. Prior to the collection of data, informed consent was taken from each and every individual.
Result
Data from 246 breast cancer patients revealed the following information. Among the total respondents, 28.8% (68) were less than 40 years of age at diagnosis while the remaining 71.2% (178) were more than 40 years of age and the mean age being 44.6 years. Regarding the education level, more than 1/3rd i.e.38.6% (95) were illiterate while only 6.1% (1%) were graduate and above. The mean monthly family income was Nrs. 13,000/-. Majority of the respondents were housewife (71.2%) and the least were government workers (10.2%). Among the respondents, 80.10% (197) were married, 14.7% (36) widowed followed by 5.3% (13) unmarried which is shown in table 1.
Table 1: Socio-demographic characteristics
|
Socio demographic factors |
Frequency |
Percentage |
Mean (SD) |
|---|---|---|---|
|
Age at diagnosis |
|||
|
<40 years |
68 |
28.8 |
44.6 (8.9) |
|
≥40 years |
178 |
71.2 |
|
|
|
|
|
|
|
Education level |
|
|
|
|
Illiterate |
95 |
38.6 |
|
|
Can only sign |
65 |
26.4 |
|
|
Primary education |
42 |
17.1 |
|
|
High school |
29 |
11.8 |
|
|
Graduate and above |
15 |
6.1 |
|
|
|
|
|
|
|
Occupation status |
|||
|
Housewife |
175 |
71.2 |
|
|
Government worker |
25 |
10.2 |
|
|
Private sector |
46 |
18.6 |
|
|
|
|
|
|
|
Marital status |
|||
|
Married |
197 |
80.1 |
|
|
Unmarried |
13 |
5.3 |
|
|
Widow |
36 |
14.7 |
|
Regarding the menopausal status, 35% were during their pre-menopausal stage while the remaining 65% were at post-menopausal stage. Regarding the first clinical presentation of breast cancer, 82.9% (204) had breast lump as the first symptom followed by nipple problems 4.9% (12) and 1.6% (4) no symptoms which is illustrated in table 2.
Table 2: Clinical presentation of breast cancer
|
Clinical characteristics |
Frequency |
Percentage |
|---|---|---|
|
Location of tumor |
||
|
on right breast |
173 |
70 |
|
on left breast |
73 |
30 |
|
|
||
|
Breast cancer output |
||
|
First breast cancer on one breast |
231 |
93.9 |
|
Second breast cancer on contra lateral breast |
15 |
6.1 |
|
|
|
|
|
First symptoms |
||
|
Breast lump |
204 |
82.9 |
|
Nipple problems |
12 |
4.9 |
|
Breast pain |
11 |
4.5 |
|
Change of breast shape |
7 |
2.8 |
|
No symptoms |
4 |
1.6 |
|
others |
8 |
3.3 |
Representation of the past medical history resulted that more than 1/3rd i.e.36.2% (89) had comorbid chronic diseases (Diabetes Mellitus, Hypertension etc.) and family history of breast cancer was found to be 19.5% (48). Regarding the hormone receptor status of the respondents, it was found that estrogen and progesterone receptors were maximum, accounting for 45.5% (112) and 43.9% (108) respectively. Whereas maximum i.e. 47.6% (117) has not received HER2/neu hormone followed by 39% (96) who had received. This information is shown in table 4.
Table 3: past medical history and hormone receptor status
|
Past medical history |
||
|---|---|---|
|
Medical history |
Frequency |
Percentage |
|
Family history of breast cancer |
48 |
19.5 |
|
History of benign breast disease |
80 |
32.5 |
|
Co-morbid chronic disease (Diabetes mellitus, Hypertension etc.) |
89 |
36.2 |
|
Hormone receptor status |
||
|
Hormone receptor |
Frequency |
Percentage |
|
Estrogen receptor |
||
|
Positive |
112 |
45.5 |
|
Negative |
98 |
39.8 |
|
Not known |
36 |
14.6 |
|
|
|
|
|
Progesterone receptor |
|
|
|
Positive |
108 |
43.9 |
|
Negative |
96 |
39.0 |
|
Not known |
42 |
17.1 |
|
|
|
|
|
HER2 new |
|
|
|
Positive |
96 |
39 |
|
Negative |
117 |
47.6 |
|
Not known |
33 |
13.4 |
The findings revealed that 44% of the respondents was at the stage III of breast cancer during the diagnosis while only 5% were at the I stage. 13% were at the last stage i.e. stage IV which is shown in figure I.
Figure I: stages of breast cancer
The graph below (Figure II) represents the percentage of presentation time for the diagnosis of breast cancer. It shows that, the majority i.e. 30.4% of the patients were diagnosed with breast cancer after 3-6 months of the symptoms appeared while 5.3% were diagnosed with a month period.
Figure II: Percentage of presentation time
We performed the multiple logistic regression to identify the significant association with various factors with delay in presentation, illustrated in table 4. From this, we revealed that the odds of delay in presentation was 4.5 times more (COR=4.56 at 95% CI: 2.32-12.2) in those who opt for alternative therapy (Ayurvedic, Homeopathy etc.) compared to those who do not go for alternative medicine. On the other hand, significant association was found regarding the factor "feeling of hesitation" which resulted that those who hesitate to share their cancer status with others were 5.71 times (COR=5.71 at 95% CI: 1.33-2.04) more prone to delay in presentation compared to those who do not hesitate. Another factor contributing towards delay was the religious value. People who have the belief that "cancer is a minor illness and god will cure it" are 4.5 times (COR=4.51 at 95% CI: 1.92-10.46) more likely for the delay compared to those who do not have such religious belief.
Economic status was also found significantly associated with delay in presentation of breast cancer. People with low economic status were 6.26 times (COR=6.26 at 95% CI: 3.61-13.39) more susceptible towards the delay in presentation of breast cancer compared to those counterparts who were in higher economic status. Another strong relationship was found with the knowledge factor as those who lack knowledge about cancer tend to be 7.32 times more (COR=7.23 at 95% CI: 4.12-15.35) prone to delay in presentation compared to those who have knowledge about cancer. Attitude towards treatment was found to have a significant association with delay in presentation as those with negative attitude have 5.91 times (COR=5.91 at 95% CI: 3.56-9.86) more tendency of delay in presentation than those having positive attitude.
Table 4: Association with various factors towards delay in presentation (multiple logistic regression model)
|
Associated factors |
Response |
Frequency |
Crude odds ratio (95% CI) |
p-value |
|
|---|---|---|---|---|---|
|
Non- delay (N=88) |
Delay (N=158) |
||||
|
Alternate therapy (Ayurvedic, Homeopathy etc.) |
Yes |
59 (68%) |
110 (69.6%) |
4.56 (1.32-12.2) |
<0.05 |
|
No |
29 (32%) |
48 (30.4%) |
Ref |
||
|
Feeling of hesitation |
Yes |
76 (86.4%) |
129 (81.6%) |
5.71 (1.33-2.04) |
<0.05 |
|
No |
12 (13.6%) |
29 (18.4%) |
Ref |
||
|
Religious value |
Yes |
70 (79.6) |
130 (82.3%) |
4.51 (1.92-10.46) |
<0.05 |
|
No |
18 (21.4%) |
28 (17.7%) |
Ref |
||
|
Low economic status |
Yes |
65 (73.9%) |
140 (88.6%) |
6.26 (3.61-13.39) |
<0.05 |
|
No |
13 (26.1%) |
18 (11.4%) |
Ref |
||
|
Lack of knowledge about cancer |
Yes |
56 (63.6%) |
146 (92.4%) |
7.23 (4.12-15.35) |
<0.05 |
|
No |
32 (36.4%) |
12 (7.6%) |
Ref |
||
|
Attitude towards treatment |
Negative |
61 (70%) |
140 (88.6%) |
5.91 (3.56-9.86) |
<0.05 |
|
positive |
17 (30%) |
28 (17.7%) |
Ref |
||
Discussion
In Nepal, breast cancer is the most prevalent cancer in women and one of the major public health problems. Also, it causes a significant add up of deaths due to the delay in their diagnosis according to Globocan 2020 (9). Research related to breast cancer has been very limited in context to Nepal. The understanding of the situation and the findings of the risk factors for the delay presentation will be helpful in improving the early diagnosis. Early stage detection is important because delay is preventable and early treatment can lead to improved survival (8). Stage at diagnosis is one of the important and independent prognostic factors determining the outcome of treatment and survival. Even the chance of recurrence and dying of metastatic disease is more when diagnosed at a higher stage.
Apart from the outcomes, there are huge financial implications for the diagnosis of breast cancer in advanced stage, both at family level and national level. In a systematic review conducted by Li Sun et al. on the global treatment cost implications of breast cancer, it was shown that the average treatment costs for stage II, III and stage IV are 32%, 95% and 109% higher than stage I.(9)
According to GLOBOCAN 2020, an estimated 1973 new breast cancer cases were diagnosed in Nepal in 2020, and recorded a death of around 1049 due to breast cancer (10). Over the last ten years Breast Cancer has been rising steadily and now it is the most common cancer in women in Nepal too. Age adjusted rate is as high as 25.8 per 100,000 women and mortality 12.7 per 100,000 women. With the advent of effective screening modalities, it is now possible to detect breast cancer at an earlier stage. Five-year survival rate of breast cancer detected at the earliest stage is more than 90% (11). Although a population-based national cancer registry does not exist in Nepal, there is a multi-institution hospital-based registry. The most common age of breast cancer patients has been reported to be 40–50 years in various population-based studies in different parts of Nepal, among which a marked proportion of Nepalese breast cancer patients were younger than 50 years of age.
The risk of breast cancer increases with age. Risk factors associated with breast cancer, including early menarche (before age 12), late menopause (after 55 years of age), nulliparity or first child birth after the age of 30 years, are similar in Asian and western populations, except for hormone replacement therapy (HRT), which is an important risk factor in Caucasians but not in Asian women (13-16). This study also correlates with the similar findings related to hormone receptor status as maximum participants were found positive towards estrogen and progesterone. While HRE neu was comparatively found less. The adoption of the westernized lifestyle of delayed childbearing, reduced breastfeeding and other westernized dietary and lifestyle patterns has a significant impact on breast cancer risk and prognosis among Asian women (17). Studies have revealed that breast cancer in premenopausal Nepalese patients was associated with late menarche (>14 years), early first full-term pregnancy (before 40 weeks of pregnancy) and a longer duration of breastfeeding, when compared with Japanese subjects (18,19). Family history is also an important risk factor for breast cancer, but there is no association between family history of breast cancer and breast cancer severity or associated mortality (20). This study also revealed that nearly 50% of the patients have a family history of breast cancer. A family history of female breast cancer in first degree relatives is reportedly rare in a Nepalese context (18). Meanwhile, studies have identified that high dietary fat, excessive alcohol intake, hormone replacement therapy, smoking and exposure to radiation may be associated with an increased risk of breast cancer in Nepalese women among other nationalities (21,22).
In this study, nearly half (44%) of patients with delayed presentation were diagnosed with III stages of breast cancer at presentation. It has been reported in studies conducted in South Africa and Ethiopia (23-25) that delayed presentation will create a good environment for the progression of the disease resulting in advanced stage diagnosis. The main reasons given by women with breast cancer for coming late to the health facility were considering the disease as nothing serious, not having enough awareness about the symptoms, and visiting a traditional healer (29). These reasons were also mentioned in other areas of the Ethiopia northwest region, Iran, Mali, Pakistan, Nigeria, and Libya (26-28).
In the present, Breast lump was a first alarm symptom in majority of our patients (82.9 %). However, women did not have sufficient background knowledge regarding this symptom and therefore the discovery of a breast lump did not reduce the patient delay which contrasted with other studies (30-32). The findings suggest that women need to be educated about the different types of breast cancer symptoms, especially the most frequent symptom as well as encouragement to seek medical advice if a symptom is ambiguous. The most frequent reasons given by women for a delayed consultation were their perception regarding the symptoms to be harmless and temporary, adding that the absence of pain cancer diagnosis remains unlikely. This demonstrates poor knowledge of our females regarding the importance of these warning signs and symptoms of breast cancer, and how much severity these symptoms can attain with the passage of time, being irreversible and even proving to be fatal in late stages. This result was consistent with a similar study conducted in Tunisia (33), in Libya (34) and in Nigeria (35).
This study also highlighted of the major factors for delay in presentation of breast cancer viz., alternate therapy (Ayurvedic, Homeopathy), feeling of hesitation towards seeking health care services, economic status, knowledge about cancer and attitude towards treatment to be significantly associated with P-value <0.05. While pursuing the alternative treatment, most patients experience worsening symptoms, which eventually lead to the delay in presentation and advance stage. The patient's interpretation of their symptoms as a sign of cancer had an important influence on whether they sought medical advice or not. Also, other studies reporting perception of risk of breast cancer have demonstrated that most women underestimate their risk to develop this disease (36). However, emotions such as fear, sadness, and worrying about diagnosis and possible treatments influence initiative to seek medical attention. So, fear has been associated with delay; it can either accelerate seeking medical attention or cause a delay. Mechanisms determining patients’ decisions are still unknown. Health system delay has been less studied in context to Nepal and research is much less. One of the main reasons is that the main medical model traditionally attributes health issues and paucity of attention to the patients without considering the influence of social and structural factors and inequity, which conditions to a differential distribution of disease, quality of attention, and health care access (37,38).
Associated factors have established that some characteristics might be younger age and presenting unspecific symptoms, both make it harder for the physician to achieve a diagnosis. Socioeconomic level as a factor for medical team delay remains controversial; perhaps, it has not been studied properly because of its effect on accessibility and acceptability of the health system, and this would be responsible for the inequity suffered by minorities and vulnerable population. Studies from different countries have estimated a global delay in breast cancer of 17% (36) in a specific population in Germany to up to 42.5% (37) in a regional hospital sample in Tehran, Iran.
This study revealed that economic status was also found significantly associated with delay in presentation of breast cancer. People with low economic status were 6.26 times (COR=6.26 at 95% CI: 3.61-13.39) more susceptible towards the delay in presentation of breast cancer compared to those counterparts who were in higher economic status. This might be due to the reason that people of higher economic status have money for their checkup at any time and do their check up on a regular basis. Many such people do their annual health package test too which is beneficial to detect the cancer at an early stage. Studies have repeatedly demonstrated that irrespective of their socio-economic and educational backgrounds, Nepalese women had poor knowledge of the risk factors of breast cancer (38,39). Although age, education, household income and family history of breast cancer are reported to be significantly with awareness level, a study on breast cancer literacy among higher secondary students demonstrated that students had poor knowledge on breast cancer risk factors, symptoms and curability (38) A cross-sectional study conducted at KIST medical college in Kathmandu revealed that 70% of the participants had never heard of breast cancer (39,40).
This study demonstrated that awareness and understanding of breast cancer among Nepalese women was notably poor. Nepalese women need to be aware of modifiable and non-modifiable risk factors of breast cancer to adopt appropriate practices for prevention. Cancer literacy provided by healthcare settings should be increased to ensure this knowledge becomes more widespread amongst the general public. The government should also formulate formal policies for effective nation- and district-wide cancer literacy programs, as well as engagements with all the three tiers of government i.e. federal, provincial and local along with the international organizations and the healthcare system. Additionally, breast health education sessions, guidance by nurses on breast self-examination, regular follow-up by nurses and other healthcare training institutions should be carried out throughout the country. An awareness campaign could be conducted through advertisements on breast cancer and screening via radio, internet, television and poster platforms to promote an attitude change regarding breast cancer in women. There is also a need to strengthen the cancer-related curriculum in medical schools, with focus on breast cancer awareness and screening methods. Furthermore, future research should continue to focus on the genetic makeup of breast cancer, to further improve understanding on the early onset of breast cancer in Nepal and other regions.
Conclusion
In conclusion, the delay in breast cancer has been a very serious problem in Nepal and other developing countries. These delays were influenced by a complex interaction of various factors and the overall perspectives for breast cancer are notably variable among women in Nepal. Factors responsible for the general delayed diagnosis were, use of alternative therapy, cultural restrictions, feeling of hesitation to share with others, lack of knowledge about cancer, negative attitude towards treatment. The study results do provide some understanding on the topic and found that almost all of those factors demonstrate a deficiency of sufficient knowledge, information and awareness in our population regarding this fatal disease. Diagnosis in early stage has huge implications on outcomes, financial burden at individual and national level. We could not alter the biological behavior of disease, but we made an attempt to identify factors which are modifiable for early diagnosis of Breast cancer in Nepal. Nepalese women need more education on breast cancer especially those at higher risk of diagnosis delay, imparting adequate knowledge to its presenting signs and symptoms, and also the necessity of regular self-breast examination. Government should foster novel policies to establish effective nationwide cancer literacy programs, as well as engagements with community-level, national and international organizations and the healthcare system as well as specific attention should be conducted to increase the awareness among general practitioners for improving breast cancer prognosis by early diagnosis and treatment.
Data availability statement Not Applicable
Acknowledgement: Authors would like to express our deepest gratitude to Institutional Review Committee of Patan Academy of Health Sciences, HAMS Hospital and B&B Hospital for their generous support and feedback.
Ethics statement Each and every participant were given full rights for the enrollment in the survey via. ethical consent form and also to withdraw at any point of time during the survey.
Funding No funding available.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136: E359–86.
2. Winters S, Martin C, Murphy D, Shokar NK. Breast cancer epidemiology, prevention, and screening. Progress in molecular biology and translational science. Amsterdam: Elsevier Inc; 2017. p. 1–32.
3. Gangane N, Anshu, Manvatkar S, Ng N, Hurtig AK, Sebastian MS. Prevalence and risk factors for patient delay among women with breast cancer in rural India. Asia Pacific Journal of Public Health. 2016;28(1):72-82.
4. Ben-EltrikiM, Deb S, Guns ES. Calcitriol in combination therapy for prostate cancer: Pharmacokinetic and pharmacodynamic interactions. J Cancer. 2016;7(4):391-5.
5. Agarwal G, Ramakant P. Breast Cancer Care in India: The Current Scenario and the Challenges for the Future. Breast Care (Basel) 2008;3:21–27. doi: 10.1159/000115288.
6. Singh YP, Sayami P. Management of breast cancer in Nepal. JNMA J Nepal Med Assoc. 2009;48:252–257.
7. Nosarti C, Crayford T, Roberts JV, Elias E, McKenzie K, David AS. Delay in presentation of symptomatic referrals to a breast clinic: patient and system factors. Br J Cancer. 2000;82:742–8.
8. Johansson AL, Trewin CB, Fredriksson I, Reinertsen KV, Russnes H, Ursin G. In modern times, how important are breast cancer stage, grade and receptor subtype for survival: a population-based cohort study. Breast Cancer Research. 2021 Dec;23:1-0.
9. Sun L, Legood R, dos-Santos-Silva I, Gaiha SM, Sadique Z (2018) Global treatment costs of breast cancer by stage: A systematic review. PLoS ONE 13(11): e0207993. https://doi.org/10.1371/journal.pone.0207993
10. Meechan G, Collins J, Petrie KJ. The relationship of symptoms and psychological factors to delay in seeking medical care for breast symptoms. Prev Med. 2003;36:374–8.
11. GLOBOCAN, corp-author. Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2020. 2012. [Jan 25;2020 ].
12. NCHRC, breast cancer text. Oncology and its incidence, prevalence, morbidity and mortality. www.nch.com.np.
13. Pradhananga KK, Baral M, Shrestha BM. Multi-institution hospital-based cancer incidence data for Nepal: An initial report. Asian Pac J Cancer Prev. 2009;10:259–262. [PubMed] [Google Scholar]
14. Binu V, Chandrashekhar T, Subba S, Jacob S, Kakria A, Gangadharan P, Menezes RG. Cancer pattern in Western Nepal: A hospital based retrospective study. Asian Pac J Cancer Prev. 2007;8:183–186. [PubMed] [Google Scholar]
15. Moore MA, Ariyaratne Y, Badar F, Bhurgri Y, Datta K, Mathew A, Gangadharan P, Nandakumar A, Pradhananga KK, Talukder MH, et al. Cancer epidemiology in South Asia - past, present and future. Asian Pac J Cancer Prev. 2010;11(Suppl 2):49–66. [PubMed] [Google Scholar]
16. Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, Hirunpat S, Woodtichartpreecha P, Boonlikit S, Teerawattananon Y, et al. Risk factors of breast cancer: A systematic review and meta-analysis. Asia Pac J Public Health. 2013;25:368–387doi: 10.1177/1010539513488795. [PubMed] CrossRef] [Google Scholar]
17. Aich RK, Mondal NK, Chhatui B, Sepai HM, Aich R, Acharyya A, Manir K, Bhattacharaya J. Relevance of risk factors of breast cancer in women: An Eastern Indian scenario. J Cancer Res Ther. 2016;12:302–308. doi: 10.4103/0973-1482.160929. [PubMed] [CrossRef] [Google Scholar]
18. Collaborative Group on Hormonal Factors in Breast Cancer, corp-author. Menarche, menopause, and breast cancer risk: Individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. Lancet Oncol. 2012;13:1141–1151. doi: 10.1016/S1470-2045(12)70425-4. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
19. 18. Porter P. “Westernizing” women's risks? Breast cancer in lower-income countries. N Engl J Med. 2008;358:213–216. doi: 10.1056/NEJMp0708307. [PubMed] [CrossRef] [Google Scholar]
20. Bhattacharya S, Adhikary S. Evaluation of risk factors, diagnosis and treatment in carcinoma breast-a retrospective study. Kathmandu Univ Med J (KUMJ) 2006;4:54–60. (KUMJ) [PubMed] [Google Scholar]
21. Singh Y, Sayami P, Sayami G, Nakagawa H, Koreeda T, Hatano T, Tsubura A. Nepalese breast cancer in relation to reproductive factors: Comparison between Nepalese and Japanese cases. Anticancer Res. 2002;22(1A):1–323. [PubMed] [Google Scholar]
22. Melvin JC, Wulaningsih W, Hana Z, Purushotham AD, Pinder SE, Fentiman I, Gillett C, Mera A, Holmberg L, Van Hemelrijck M. Family history of breast cancer and its association with disease severity and mortality. Cancer Med. 2016;5:942–949. doi: 10.1002/cam4.648. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
23. Gram IT, Park SY, Kolonel LN, Maskarinec G, Wilkens LR, Henderson BE, Le Marchand L. Smoking and Risk of Breast Cancer in a Racially/Ethnically Diverse Population of Mainly Women Who Do Not Drink Alcohol: The MEC Study. Am J Epidemiol. 2015;182:917–925. doi: 10.1093/aje/kwv092. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Tara S, Agrawal CS, Agrawal A. Validating breast self examination as screening modalities for breast cancer in eastern region of Nepal: A population based study. Kathmandu Univ Med J (KUMJ) 2008;6:89–93. [PubMed] [Google Scholar]
25. Tesfaw A, Demis S, Munye T, Ashuro Z. Patient delay and contributing factors among breast cancer patients at two cancer referral centres in Ethiopia: a Cross-Sectional Study. J Multidiscip Healthc. 2020;13:1391. doi: 10.2147/JMDH.S275157.
26. Harirchi I, Karbakhsh M, Hadi F, Madani SS, Sirati F, Kolahdoozan S. Patient delay, diagnosis delay and treatment delay for breast cancer: comparison of the pattern between patients in public and private health sectors. Arch Breast Cancer. 2015:52–57.
27. Khan MA, Hanif S, Iqbal S, Shahzad MF, Shafique S, Khan MT. Presentation delay in breast cancer patients and its association with sociodemographic factors in North Pakistan. Chin J Cancer Res. 2015;27(3):288. doi: 10.3978/j.issn.1000-9604.2015.04.11 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Ibrahim N, Oludara M. Socio-demographic factors and reasons associated with delay in breast cancer presentation: a study in Nigerian women. Breast. 2012;21(3):416–418. doi: 10.1016/j.breast.2012.02.006 [PubMed] [CrossRef] [Google Scholar]
29. Grosse Frie K, Kamaté B, Traoré CB, et al. Factors associated with time to first healthcare visit, diagnosis and treatment, and their impact on survival among breast cancer patients in Mali. PLoS One. 2018;13(11):e0207928. doi: 10.1371/journal.pone.0207928 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
30. Ermiah E, Abdalla F, Buhmeida A, Larbesh E, Pyrhönen S, Collan Y. Diagnosis delay in Libyan female breast cancer. BMC Res Notes. 2012;5(1):1–8. doi: 10.1186/1756-0500-5-452 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Harirchi I, Karbakhsh M, Hadi F, Madani SS, Sirati F, Kolahdoozan S. Patient delay, diagnosis delay and treatment delay for breast cancer: comparison of the pattern between patients in public and private health sectors. Arch Breast Cancer. 2015:52–57. [Google Scholar]
32. Ramirez AJ, Westcombe AM, Burgess CC, Sutton S, Littlejohns P, Richards MA. Factors predicting delayed presentation of symptomatic breast cancer: a systematic review. Lancet. 1999;353(9159):1127–31
33. Montella M, Crispo A, Botti G, De Marco M, De Bellis G, Fabbrocini G, et al. Assessment of delay in obtaining definitive breast cancer treatment in southern Italy. Breast Cancer Res Treat. 2001;66:209–15.
34. assem J, Ozmen V, Bacanu F, Drobniene M, Eglitis J, Lakshmaiah KC, Kahan Z, Mardiak J, Pie?kowski T, Semiglazova T, Stamatovic L,Timcheva C, Vasovic S, Vrbanec D, Zaborek P. Delays in diagnosis and treatment of breast cancer: a multinational analysis. Eur J Public Health. 2013;12:1–7.
35. Landolsi A1, Gahbiche S, Chaafii R, Chabchoub I, Ben Fatma L, Hochlef M, Gharbi O, Ben Ahmed S. Reasons of diagnostic delay of breast cancer in Tunisian women (160 patients in the central region of Tunisia). Tunis Med. 2010;88(12):894–7
36. Ermiah E, Abdalla F, Buhmeida A, Larbesh E, Pyrhönen S, Collan Y. Diagnosis delay in Libyan female breast cancer. BMC Res Notes. 2012;5:452.
37. Ukwenya AY, Yusufu LM, Nmadu PT, Garba ES, Ahmed A. Delayed treatment of symptomatic breast cancer: the experience from Kaduna, Nigeria. S Afr J Surg. 2008;46(4):106–1
38. Arndt V, Sturmer T, Stegmaier C, Ziegler H, Dhom G, Brenner H. Patient delay and stage of diagnosis among breast cancer patients in Germany—a population based study. Br J Cancer. 2002;86:1034–1040.
39. Harirchi I, Ghaemmaghami F, Karbakhsh M, Moghimi R, Mazaherie H. Patient delay in women presenting with advanced breast cancer: an Iranian study. Public Health. 2005;119:885–891.
40. Sathian B, Nagaraja SB, Banerjee I, Sreedharan J, De A, Roy B, Rajesh E, Senthilkumaran S, Hussain SA, Menezes RG. Awareness of breast cancer warning signs and screening methods among female residents of Pokhara valley, Nepal. Asian Pac J Cancer Prev. 2014;15:4723–4726. doi: 10.7314/APJCP.2014.15.11.4723.
41. Shrestha K. Breast cancer knowledge and screening practice among women visited to KIST medical college. Nepal Med Coll J. 2012;14:308–311. [PubMed] [Google Scholar] [Ref list]
42. Bhandari PM, Thapa K, Dhakal S, Bhochhibhoya S, Deuja R, Acharya P, Mishra SR. Breast cancer literacy among higher secondary students: Results from a cross-sectional study in Western Nepal. BMC Cancer. 2016;16:119. doi: 10.1186/s12885-016-2166-8. [PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list].
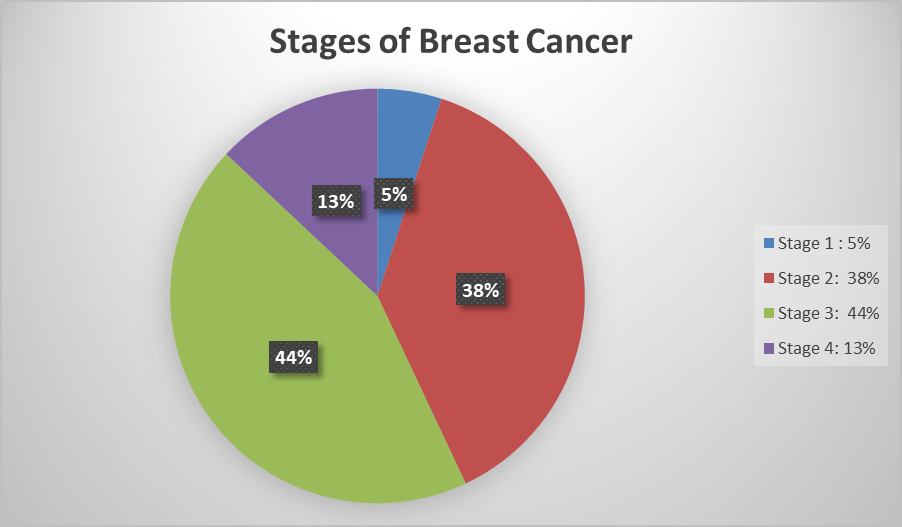
Figure 1
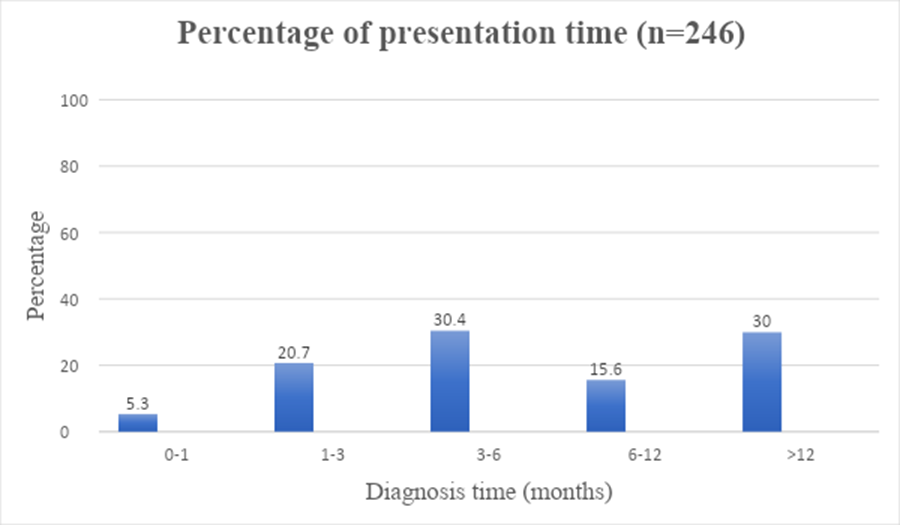
Figure 2
