The Laparoscopic Dermoid Cystectomy Suspected Challenges how to Overcome it
The Laparoscopic Dermoid Cystectomy Suspected Challenges how to Overcome it
Salma Gerais *1, Ismaeil Salim Ismaeil 2, Hilmi Daoud Elsiddig Elazhari 3, Arwa A.E. Musa
*Correspondence to: Salma Gerais.
Copyright
© 2024 Salma Gerais. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 22 July 2024
Published: 01 August 2024
The Laparoscopic Dermoid Cystectomy Suspected Challenges how to Overcome it
Introduction
Germ cell tumors are derived from germ cells and account for 30 percent of ovarian tumors. Furthermore, mature cystic teratomas are the most common ovarian germ cell tumor. Teratomas are composed of tissues derived from two or three embryonic layers (i.e ectoderm, mesoderm and endoderm) which maybe manifested as hair, teeth, muscle or bone [1]. Due to their high incidence in females and the risk of ovarian torsion, it is essential for them to be removed through surgical laparoscopy [2].
Case Report
A 29 years old female presented with a chief complaint of right iliac fossa pain.
Pelvic ultrasound showed a left dermoid ovarian cyst. The abdominal MRI pelvis with contrast showed a mass lesion of about 12.5cm vertically, 11.5cm TS and 10cm in AP diameter in the cul de sac space, encapsulated in tough capsule and consist of fluid signals, soft tissue and fat signals with some tiny foci of very low signal intensity on all pulse sequences which may stand for calcification. All the serum tumor markers were normal.
Fig 1.1: Sagittal view
Fig 1.2: Horizontal view
Fig 1: Preoperative abdominopelvic Magnetic resonance imaging with contrast demonstrating a mass lesion of about 12.5cm vertically ,11.5cm TS and 10cm in AP diameter in the cul de sac space, encapsulated in tough capsule; consist of fluid signals, soft tissue, fat signals and calcifications.
Fig 2: Dermoid cyst, showing hairs +sebaceous material
A laparoscopic ovarian cystectomy was done under general anesthesia on 15/2/2022. Intra operatively, the cyst was ruptured with the spillage of some of the content inside the abdomen, a wash was done, the contents was inserted inside the endo bag and removed through the primary port entry. The bag was full of hair and fatty material, the content was sent for histopathology.
Fig 3: (A) Histopathology of the cyst showing low power view of the cyst wall epidermal and dermal elements. (B),(C) Microcalcifications
The histopathology report confirmed the diagnosis of Mature cystic teratoma Fig 3.
The patient was monitored for 24 hours postoperatively, course was uneventful. On postoperative day number six she presented with fever, Nausea, vomiting and Right upper quadrant pain.
The patient was admitted to the hospital due to concerns of postoperative sepsis. All the septic parameters were raised including total white blood cell count, lactate, C-reactive protein (CRP) and her Hemoglobin dropped. She received two units of blood, intravenous antibiotics, prophylactic anticoagulant, iv fluids and anti-pyretic.
The site of Left trocar was oozing serosanguinous fluid,an incision was made and a collection was removed, sent to cytology, culture and sensitivity. The results showed no growth. Repeat Pelvic US showed residual collection.
The abdominal pain persisted along with Tachycardia and Tachypnea. A CT abdomen and pelvis with contrast showed a moderate amount of pelvic ascites that contain debris and densities with questionable hemorrhage. The outlines of uterus was preserved, no free intraperitoneal air. The patient was evaluated by surgeon he excluded the suspicion of bowel injury. CT guided aspiration was done, Drain was placed and 100 ml fluid was removed from the right iliac fossa, specimen was sent for cytology, culture and sensitivity the result showed no growth. Hospital course was then complicated by AKI, nephrology was consulted, managed with fluids, Lasix, avoiding nephrotoxins, kidney function returned back to normal.
The patient then developed diarrhea along with continued abdominal pain, persistent leukocytosis, thrombocytosis, worsening creatinine and fluid analysis was consistent with exudative features. The decision was taken to go for urgent laparotomy.
Fig 4.1: High power view of a section from cell block prepared from ascitic fluid.
Clumps of degenerate red cells and neutrophils are seen
Fig 4.2: Small bowel was matted (pseudo obstruction)
A lower midline incision was performed, a small bowel was matted together with scattered adhesion (pseudo obstruction), chemical irritant + feature of peritonitis, a small collection was found in the pouch of Douglas. No perforation no hematomas. Scattered hairy materials was removed, A wash with warm saline was done, two drains were inserted. Her Clinical status improved dramatically.
On Postoperative day four, she developed chest pain and tachycardia. ECG showed sinus tachycardia with concerns of RV strain, her d dimer was raised, CTPA was deferred due to her recent AKI. She was admitted to the HDU and started on Therapeutic anticoagulation as an empirical treatment of Pulmonary embolism and for possible atelectasis. Chest X ray showed feature of Rt side pleural effusion. A pleural tab was done and sent for culture and sensitivity, results showed no growth. The clinical symptoms and signs improved, inflammatory markers trended down and patient was discharged home on Therapeutic anti-coagulant + intravenous antibiotics. After completing her antibiotics, she was seen in the office for follow up, complaining of severe generalized joint pain fever. Antibiotics duration was extended.
She again developed high grade fever. Fluid collection was noted at site of primary trocar, it was drained, Labs were collected, it was significant for leukocytosis, thrombocytosis and drop in hemoglobin, with raised CRP and negative procalcitonin. She received Packed RBCs and antibiotics with no clinical improvement. internal medicine physician was consulted, ANA profile was sent and she was started on steroids as per rheumatology. She received 40 mg of prednisolone, tapered by 10 mg every 7 days for one month.
Her clinical symptoms, appetite and oral intake improved along with normalization of her lapse.
Discussion
Meticulous dissection of the cyst and use of endo bag is beneficial to remove the cyst through the port site [3]. If spillage of contents is suspected, irrigation and changing patient position to the reverse Trendelenburg will help spilled contents flow downward from the upper abdomen [4]. If the spillage occurs following saline irrigation a drain insertion is recommended. If there clinical evidence of chemical peritonitis or suspicion of bowel obstruction Urgent laparotomy with peritoneal lavage and removal of remaining dermoid cyst contents should be performed as soon as possible.
This case was challenging to manage as the patient’s symptoms and signs improved transiently after the urgent laparotomy. Shortly thereafter, clinical symptoms &signs of sepsis/inflammatory response emerged including raised total TWBCS, platelets and CRP with a drop in the Hemoglobin level. Given her persistent symptoms despite antibiotics, negative infectious work up, steroids were administered. The role of steroids in the treatment of the symptoms was obvious with normalization of the blood parameters. As per literature review, we identified a case of chemical peritonitis secondary to spontaneous ruptured dermoid cyst [5] managed with drain, laparotomy and steroids However in the case described by H.S Yang rupture was spontaneous and steroids were started earlier in the hospital course. Another case reported by Reiko TASKA of spontaneous rupture of an ovarian mature cystic teratoma, complete removal of the cyst content was unsuccessful due to the high risk of intestinal injury. The patient received hydrocortisone followed by oral prednisolone for one year, no symptoms of chemical peritonitis recurred [6].
Conclusion
This case highlights the significance of multidisciplinary approach in managing of chemical peritonitis secondary to ruptured dermoid cyst including urgent laparotomy and peritoneal lavage, ruling out bacterial infections and assessing the need to use steroids. In our case, steroids were found to be effective in alleviating the patient clinical symptoms and reduced inflammatory markers after exclusion of bacterial infection.
References
1.Sudha Sunder,( 2016 ).p889 , Obstetrics & gynaecology an Evidence base Text m third edition .
3. Hyo-Eun Kim ,minji seo ,Jae young kwack , YONG-soon Kwon,Granulamatous pertonities caused by iatrogenic spillage of ovarian dermoid cystectomy :a case report and literature review,obstet Gynecol Sci 2020:63(4):543-547,published online 19 June 2020.DOI:http//doi.org/10.5468/ogs.19189.
4. Clement D, barranger E ,Benchimol Y.Uzan S .Chemical peritonitis : a rare complication of an iatrogenic ovarian dermoid cyst rupture .Surg Endosc.2003;17:658.
5. Hyun Sung Yang, MD1, Tae Hun Song, MD1, Hyun Chul Bang, MD1, Jun-Ho Park, MD1, Chae Hyeong Lee, MD1, Ju-Won Roh, MD, PhD1, Eo-Jin Kim, MD, PhD2, Yong Seok Lee, MD, PhD3, Seung-Su Han, MD4 https://synapse.koreamed.org/upload/synapsedata/pdfdata/2021kjog/kjog-54-726.pdf
6. Reiko Tasaka Sucessful treatment of severe chemical peritonitis caused by spontaneous rupture of an ovarian mature cystic teratoma using corticosteroid a case report published in Advanced in Obstetrics and Gynecology 2013 volume 65 issue 2 page 153-160. https://doi.org/10.11437/spanpunosinpo.65.153.
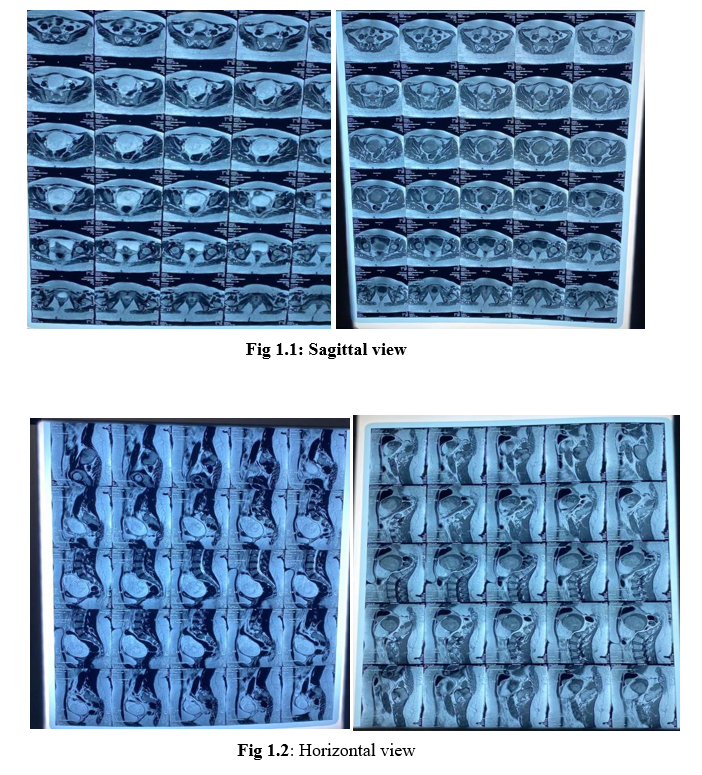
Figure 1

Figure 2
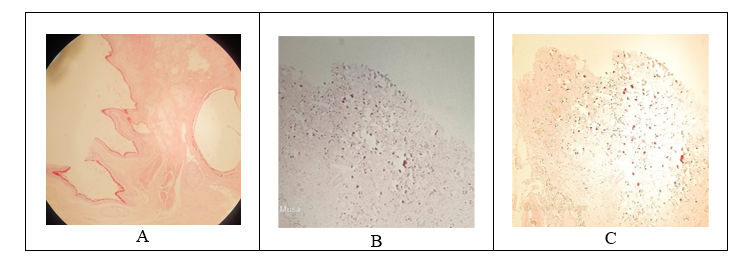
Figure 3
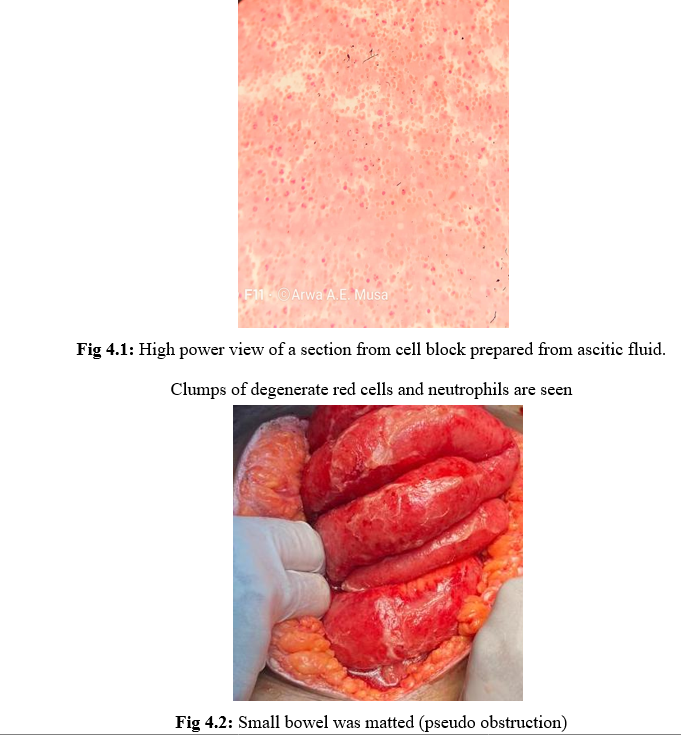
Figure 4
