Assessing the Accuracy of Ultrasound in Diagnosing Benign Ovarian Cysts and Its Impact on MRI Utilization in Infertility Management: A Retrospective Analysis
Assessing the Accuracy of Ultrasound in Diagnosing Benign Ovarian Cysts and Its Impact on MRI Utilization in Infertility Management: A Retrospective Analysis
Wilson Lim1, Seema Karan2, Panayoti Bachkangi1,3 *
1.University Hospitals of Derby and Burton NHS Foundation Trust
2. Northern Lincolnshire and Goole NHS Foundation Trust
3. University of Leicester
*Correspondence to: Panayoti Bachkangi. University Hospitals of Derby and Burton NHS Foundation Trust, University of Leicester.
Copyright
© 2024 Panayoti Bachkangi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 08 August 2024
Published: 21 August 2024
Assessing the Accuracy of Ultrasound in Diagnosing Benign Ovarian Cysts and Its Impact on MRI Utilization in Infertility Management: A Retrospective Analysis
Introduction
The accurate diagnosis of benign ovarian cystic lesions is crucial in the management of patients, particularly those undergoing infertility investigations. Ultrasound (US) is primary imaging modality employed for this purpose due to its accessibility, cost-effectiveness, and non-invasive nature. However, its reliability in differentiating simple benign cysts from complex or possibly malignant ones remains a challenge. Accurate initial diagnoses are crucial to prevent unnecessary follow-up magnetic resonance imaging (MRI), which is more resource intensive.
Current standard of practice by The Royal College of Obstetricians and Gynaecologists (RCOG) recommends pelvic ultrasound imaging, particularly transvaginal ultrasound as the first line and most effective imaging modality for evaluating adnexal masses, with MRI reserved for indeterminate or complex masses.[1]
The aim of this study was to determine whether the initial US diagnoses were accurate enough to avoid the need for further MRI assessment.
Material and Methods
The study was a retrospective analysis of MRI reports undertaken over a five-month period, from January 2023 to May 2023. Reports were retrieved form IMPAX/Xero. Ethical approval was not indicated as the project was a service evaluation and all the data anonymous. The analysis focused on MRI report texts that included ovarian cysts to assess the accuracy of initial ultrasound diagnoses. Ethical approval was not required as our study was classified as an audit.
55 MRI cases reporting ovarian cysts were identified. The selection criteria were narrowed to include only simple, benign, functional, physiological, and polycystic ovarian syndrome (PCOS) cysts. Most of them while being investigated for infertility, where cysts were incidental findings, or where the MRI was performed for surgical purposes, such as for known endometriotic cysts, were excluded. This resulted in the exclusion of 31 cases. The final analysis included 24 MRIs conducted following ultrasound reports indicating complex ovarian cysts for patient under infertility investigation.
Results
Of the 24 MRI cases analysed, 17 cases (71%) revealed simple benign cysts, while 7 cases (29%) involved a mixture of complex but benign and malignant cysts (Figure 1). The age proved not to be a significant factor between the included and excluded patients (Mann-Whitney U Test, p= 0.362) or among the included patients with simple cysts and those with complex ones (Mann-Whitney U Test, p= 0.727).
These findings indicate that over 70% of the MRI scans performed due to ultrasound reports of complex ovarian cysts were unnecessary, as the cysts were ultimately found to be simple and benign. This significantly falls short of the 100% accuracy target, highlighting the limitations of current ultrasound diagnostic practices [1].
Figure 1: MRI scans included in the study. Out of the 24 cases 17 turned to be simple and benign, while 7 were either complex benign or malignant.
Discussion
The impact of ovarian cysts on infertility is debated. Simple cysts are usually benign and functional, posing no threat to fertility [2]. Unlike endometriomas and dermoid cysts, which can affect ovarian reserve and thereby impact fertility [3,4]. Moreover, a simple adnexal cyst does not raise the risk of malignancy in women of average risk, irrespective of their menopausal status[5]. This distinction is crucial as it informs clinical decision-making, especially in infertility investigations where the preservation of ovarian function is paramount. Moreover, women with simple cysts can be reassured about their benign nature, reducing anxiety and the need for extensive follow-up.
Surgical treatment often poses a greater risk to ovarian reserve than the cyst itself [2]. Additionally, surgery does not appear to enhance pregnancy rates. Surgical interventions, while sometimes necessary, can lead to a reduction in ovarian reserve. Shandley LM at al. reported women who had undergone ovarian cyst surgery were more likely to report a history of infertility compared to age-matched women with no history of cyst surgery, although it could be both the surgical removal of ovarian cysts and the underlying conditions that necessitate such surgeries may influence a woman's ability to conceive successfully [6]. Another study also suggested that excision of ovarian dermoid cysts can significantly diminish ovarian reserve, much like the cyst itself. However, the presence or removal of dermoid cysts does not impact key IVF outcomes [4]. Therefore, it is essential to accurately diagnose and differentiate benign cysts to avoid unwarranted surgical procedures. Moreover, counselling patients prior to the surgical treatment of cysts is of utmost importance. Patients should be informed about the nature of their cysts, the risks associated with surgery, and the potential impact on fertility [7]. Proper counselling ensures that patients can make informed decisions about their treatment options, potentially opting for less invasive management strategies when appropriate.
Undoubtedly, MRI has more superior imaging capabilities as compared to US, to facilitate a more detailed evaluation of cystic structures, aiding in accurate diagnosis and appropriate management. However, a recent large community-based setting study showed that MRI has limited role in differentiating benign and malignant cases, which it only identified 16.7% of true malignant cases [8]. This has further strengthened the need for better enhancement in ultrasound diagnostic protocols and training such as IOTA simple rules.
Conclusion
The study reveals a substantial gap in the accuracy of ultrasound for diagnosing simple benign ovarian cysts. With an accuracy rate of only 71%, there is a clear need for improved diagnostic practices to reduce unnecessary MRI follow-ups. Enhancing ultrasound protocols and training can lead to better diagnostic accuracy, optimizing resource use and patient care. Future research should aim to refine ultrasound techniques to achieve higher diagnostic precision, ultimately reducing the reliance on MRI and unnecessary surgical interventions.
References
1. Management of suspected ovarian masses in premenopausal women. RCOG. Green top guideline No 62 (2011)
2. Balachandren, N; Yasmin, E; Mavrelos, D; Saridogan, E; (2021) Does ovarian cystectomy pose a risk to ovarian reserve and fertility? The Obstetrician & Gynaecologist , 23 (1) pp. 28-37
3. Guillaume Legendre, Laurent Catala, Catherine Morinière, Céline Lacoeuille, Françoise Boussion, Loïc Sentilhes, Philippe Descamps, Relationship between ovarian cysts and infertility: what surgery and when?,Fertility and Sterility, Volume 101, Issue 3, 2014, Pages 608-614
4. Lei Yan, Miao Li, Bing-Qian Zhang, Xin-Xin Xu, Zhen Xu, Ting Han, Zi-Jiang Chen, Effect of ovarian dermoid cyst excision on ovarian reserve and response: Insights from in vitro fertilization, Gynecology and Minimally Invasive Therapy, Volume 5, Issue 4, 2016, Pages 161-165
5. Peter S. Wang, Otto G. Schoeck, and Mindy M. Horrow, Benign-appearing Incidental Adnexal Cysts at US, CT, and MRI: Putting the ACR, O-RADS, and SRU Guidelines All Together, RadioGraphics 2022 42:2, 609-624
6. Shandley LM, Spencer JB, Kipling LM, Hussain B, Mertens AC, Howards PP. The Risk of Infertility After Surgery for Benign Ovarian Cysts. J Womens Health (Larchmt). 2023 May;32(5): 574-582.
7. Keyhan S, Hughes C, Price T, Muasher S. An Update on Surgical versus Expectant Management of Ovarian Endometriomas in Infertile Women. Biomed Res Int. 2015; 2015: 204792.
8. Lin R, Hung YY, Cheng J, Suh-Burgmann E. Accuracy of Magnetic Resonance Imaging for Identifying Ovarian Cancer in a Community-Based Setting. Womens Health Rep (New Rochelle). 2022 Jan 31;3(1):43-48. doi: 10.1089/whr.2021.0106. PMID: 35136876; PMCID: PMC8812505
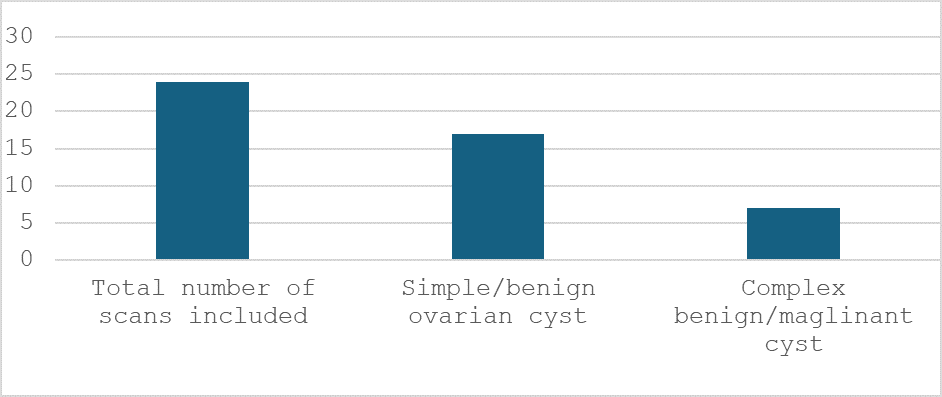
Figure 1
