Multifocal, Multicentric Osteoid Osteoma: A Rare Presentation in a 36-Year-Old Military Personnel.
Multifocal, Multicentric Osteoid Osteoma: A Rare Presentation in a 36-Year-Old Military Personnel.
Budur Alnefaie1, Abdulaziz Alnufaei2, Mohammed Alattas3, Raheef Alatassi4, Alanoud Algouaiz5
*Correspondence to: Budur Alnefaie.
Copyright
© 2024 Budur Alnefaie. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 Sep 2024
Published: 17 Sep 2024
DOI: https://doi.org/10.5281/zenodo.13772368
Abstract
This case report presents a rare instance of multifocal, multicentric osteoid osteomas in a 36-year-old male military personnel. The patient experienced progressive intermittent left leg pain for two months, with no history of trauma. Initial radiographs indicated subtle sclerosis in the left tibia, and further CT scans confirmed the presence of osteoid osteomas. A Tc-99m MDP three-phase bone scan and MRI corroborated the diagnosis, revealing multiple cortical lesions in both tibiae. The patient underwent successful radiofrequency ablation (RFA) under CT guidance, although the procedure was complicated by a second-degree burn, managed by plastic surgery, and subsequent infection with S. aureus. Histopathology confirmed the diagnosis of osteoid osteoma. Postoperative imaging showed no recurrence, and follow-up scans identified an additional lesion in the frontal bone. This case underscores the importance of comprehensive imaging for accurate diagnosis and the effectiveness of RFA in treating osteoid osteomas, while also highlighting the need for meticulous procedural planning and follow-up to manage potential complications. Future research should focus on refining diagnostic and therapeutic protocols to enhance patient outcomes.
Multifocal, Multicentric Osteoid Osteoma: A Rare Presentation in a 36-Year-Old Military Personnel.
Introduction
Osteoid osteomas (OO) are benign, predominantly solitary bone-forming tumors that make up 2-3% of primary bone tumors and 10-14% of all benign bone tumors [1]. Osteoid osteoma was first reported by Jaffe in 1935 [2]. The core of OO, known as the nidus, is the tumor itself. It is usually small, ranging in size from 1.0 to 2.0 cm, and is encircled by corticoperiosteal thickening [2, 3].
The typical clinical presentation is sporadic pain at the tumor site, which worsens at night and is relieved by nonsteroidal anti-inflammatory drugs (NSAIDs) [4, 5]. With respect to locations, the diaphysis and metaphysis of the long bones are most frequently involved in OO (approximately 50% and 40%, respectively) [6]. More than 50% of cases involve the femur and tibia, whereas the humerus may also be affected in 8% of cases affect [6, 7]. Approximately 30% of cases involve the hands, feet, and spine; OO less frequently affects the skull, scapula, pelvis, ribs, mandible, and patella [8, 9].
Computed tomography (CT) and plain radiography are typically adequate for diagnosing osteoid osteomas [10, 11]. As some tumors regress naturally over two to six years, the initial treatment is conservative and involves salicylates or NSAIDs [12-14]. If this fails, surgical intervention is needed. Today, minimally invasive methods are regarded as the gold standard of care, replacing open surgery. Techniques such as radiofrequency ablation are favored [15].
Since fewer than 1% of known cases involve multiple osteoid osteomas within a single patient, they are almost always solitary [16]. Multiple osteoid osteomas usually manifest as nidi in the same bone rather than in different bones [17]. We present a case of a patient with multifocal and multicentric tumors involving both tibia and the skull.
Case Presentation
Otherwise, healthy 36-year-old male smoker military personnel presented to the Emergency Department (ED) with a 2-month history of progressive intermittent left leg pain, primarily affecting the anterior aspect. There was no history of trauma. Physical examination and laboratory tests revealed no abnormalities except for mild tenderness at the affected site.
Radiographs taken in the ED demonstrated a lesion with subtle sclerosis in the anterolateral midshaft of the left tibia (Figure 1). A CT scan of the left leg revealed a focal cortical lesion with central calcification suggestive of an osteoid osteoma in the anterior aspect of the left mid-tibial shaft. Proximal to this lesion, another similar lesion with a periosteal reaction was noted just distal to the tibial tuberosity (Figures 2-4).
Three weeks later, a Tc-99m MDP three-phase bone scan (Figure 5) revealed focal mild hyperemia in the proximal left lower leg and intense linear hyperemia in the mid-left lower leg. Mild focal hyperemia was also observed in the right distal lower leg. Delayed planar bone phase images revealed increased tracer uptake in the proximal left tibia, midshaft of the left tibia, and distal shaft of the right tibia. The area of linear uptake along the mid-left tibial shaft corresponded to the cortical sclerotic lesion with multiple lytic nidi, indicative of 'osteoid osteoma with multicentric nidus.' SPECT-CT fused images confirmed these findings, revealing abnormal tracer uptake corresponding to multiple cortical lytic lesions (central lytic nidus with surrounding sclerosis), suggestive of multifocal osteoid osteomas involving both tibiae.
One week later, an MRI (Figure 6) of both legs revealed two cortical lesions within the midshaft of the left tibia, with enhancement and a surrounding periosteal reaction with intramedullary signal changes likely representing an osteoid osteoma. Another suspicious osteoid osteoma was noted in the proximal shaft of the left tibia and the distal shaft of the right tibia, with less enhancement and surrounding inflammatory changes.
The following day, the patient underwent radiofrequency ablation (RFA) under CT guidance for osteoid osteomas in the left tibia, accompanied by a biopsy. The procedure was complicated by 2nd-degree burns at one of the ablation sites, which were later managed by plastic surgery. During the follow-up, wound cultures from the skin lesions tested positive for S. aureus. No other complications were encountered. Histopathology of the left tibial lesion biopsy revealed thickened trabeculae of bone with adjacent loose fibrovascular stroma and prominent osteoblastic rimming, which was consistent with OO. Postoperative radiographs were taken, and they demonstreated no abnormalities (Figure 7). During the follow-up examination, another bone scan (Figure 8) was performed after the operation. A tiny focal area of abnormal tracer uptake was observed involving the frontal bone along the lateral aspect of the right orbit, which is suggestive of a frontal bone osteoid osteoma.
Figure 1a: This preoperative X-ray shows the AP view of the left tibia, revealing areas of cortical thickening indicative of osteoid osteoma. The imaging is crucial for assessing the location and extent of the lesion before surgical intervention.
Figure 1b: This preoperative X-ray shows the lateral view of the left tibia. The image highlights the cortical thickening and possible nidus characteristic of osteoid osteoma. This view complements the anterior view by providing additional information on the depth and precise localization of the lesion.
Figure 2: Preoperative Axial CT Scan of the Left Tibia. (A) This axial CT scan reveals a nidus characteristic of an osteoid osteoma in the cortex of the left tibia. The image shows a distinct round lucency with a surrounding sclerotic reaction. In addition, there was a central area of calcification. (B) Similar to the previous image, this axial CT scan further illustrates the cortical nidus associated with the osteoid osteoma. The lucent area is surrounded by reactive sclerosis, which is typical for this condition. (C) Another axial view highlighting the nidus and the surrounding sclerosis. The nidus appears as a small, well-defined radiolucent area within the thickened cortical bone
Figure 3: Preoperative Coronal CT Scan of the Left Tibia. (A) This coronal CT scan provides longitudinal view of the left tibia, clearly depicting the cortical thickening and the nidus of the osteoid osteoma, with a central calcification. The vertical extent of the lesion was well visualized. (B) A detailed sagittal view showing the vertical alignment of the lesion and the associated cortical reaction. The sclerotic area around the nidus is prominent, confirming the osteoid osteoma diagnosis. (C) Extended sagittal view further emphasizing the longitudinal spread of the osteoid osteoma lesions within the tibia. The surrounding bone sclerosis and cortical thickening are clearly evident
Figure 4: Preoperative 3D Reconstruction CT Scan of the Left Tibia. A 3D reconstruction CT scan providing a comprehensive view of the left tibia. The cortical lesion indicative of osteoid osteoma is visible, along with the surrounding bone reaction. This view aids in surgical planning and understanding the spatial relationship of the lesion within the bone structure
Figure 5a: Preoperative Bone Scan of the Legs (Anterior View). This bone scan of the legs shows increased radiotracer uptake in the left tibia, indicative of active osteoid osteoma. The localized area of increased uptake corresponds to the site of the lesion, confirming its hypermetabolic activity.
Figure 5b: Preoperative Bone Scan of the Legs (Anterior View) This posterior view of the bone scan also demonstrates increased radiotracer uptake in the left tibia, consistent with osteoid osteoma. The scan highlights the metabolic activity and helps in pinpointing the exact location of the lesion for further diagnostic and therapeutic planning
Figure 6: Preoperative MRI Scan of the Legs (Coronal View) This coronal MRI scan of the legs demonstrates the detailed soft tissue and bone structure. The image shows a hyperintense signal in the cortex of the left tibia, consistent with the presence of an osteoid osteoma. The surrounding bone marrow edema is also visible, which is typical in active lesions. This MRI provides critical information for the diagnosis and surgical planning of osteoid osteoma.
Figure 7: Postoperative X-rays. (A) AP X-ray of the left tibia showing resolution of the cortical sclerosis and periosteal reaction at the midshaft region. (B) AP X-ray of the left tibia demonstrating normal bony architecture with no signs of the previous osteoid osteoma. (C) Lateral X-ray of the left tibia showing the absence of the previously noted cortical lesions and confirming successful treatment with no recurrence.
Figure 8: Postoperative Bone Scan of the Skull. This bone scan of the skull demonstrates areas of increased radiotracer uptake, particularly in the right orbital region, as indicated by the red arrows. The scan reveals metabolic activity suggestive of a lesion, which could be consistent with an osteoid osteoma. The different views (axial, sagittal, and coronal) provide comprehensive imaging to aid in accurate localization and diagnosis of the lesion.
Case Discussion
Multiple osteoid osteomas are rare; their presence was first reported by Scehawjowicz in 1970 [18]. Typically, instead of appearing in separate bones, several osteoid osteomas manifest as nidi within the same bone [17]. De Ga K et al. reported 23 cases in which osteoid osteomas were identified within the same bone and 6 cases where they were detected in nearby bones [19]. Multicentric OO is extremely rare, with only 32 cases of OO with multiple nidi in single and multiple bones documented in the international literature thus far [20]. Multiple nidi were discovered in three different cases in two widely separated bones, six cases where they were found in bones close to each other, and 23 cases where they were found in a single bone [20]. To the best of our knowledge, our patient is one of only eight cases of multiple osteoid osteomas in two widely separated bones that have been documented in the medical literature [17, 19-20].
According to some authors, monostotic multifocal lesions result from a healing response that splits a single nidus into multiple nidi. Another theory suggests that distinct lesions could constitute a developmental stage in the potential evolution of osteoblastoma [17, 21]. Neither of these hypotheses can fully account for the pathophysiology of polyostotic osteoid osteoma. The exact causes of polyostotic osteoid osteoma and solitary osteoid osteoma remain unknown [22].
Traditionally, osteoid osteomas have been categorized into cortical, medullary (or cancellous), and subperiosteal (or periosteal) types. OO is most frequently found in the cortex [23]. In cortical locations, the central nidus is sometimes obscured by extremely dense sclerosis. Osteomas in medullary locations should appear as radiolucent or opaque zones without perifocal sclerosis [24]. In our case, the nidi of the OO within the left tibia were located in the cortex.
The only instance of multicentric synchronous anatomically separated osteoid osteomas that we are aware of was reported by Buluxc et al. [25]. Lesions were detected in the wrist, the proximal portion of the femur, and the superolateral aspect of the left orbit via a three-phase bone scan. At the time of surgery, the wrist lesion was histopathologically confirmed to be an osteoid osteoma; however, the other lesions were diagnosed by CT and not biopsied because the patient was asymptomatic. Furthermore, as far as we are aware, our patient is the first case in which there is synchronous involvement of more than two bones, each with more than one nidus [17, 19-20, 25].
Atypically located lesions, such as those in this instance on the frontal bone, can present clinically and radiologically as confusing. An incorrect diagnosis could delay treatment, leading to long-term morbidity [26]. A radiolucent nidus encircled by reactive bone can be seen on radiography [27]. The most helpful preoperative test for nidus localization is CT [20]. While increasing the spatial resolution of MR images may eventually enable better identification of the central nidus, CT remains the preferred method for diagnosing osteoid osteoma [8]. In our instance, CT, MRI, and bone scans, in addition to plain radiographs, were utilized for accurate localization, characterization of the lesion, and preoperative planning.
Persistent pain is typically the indication for osteoid osteoma treatment. Historically, surgical en bloc excision has been part of treatment. RFA was first used to treat osteoid osteomas in 1992, and since then, it has swiftly gained acceptance as a common therapeutic approach [19, 28, 29]. RFA is now widely regarded as the preferred treatment for osteoid osteomas because it is a straightforward, minimally invasive technique with 89%–95% clinical success rates [29, 30]. RFA was effective in treating lesions in our patient's left tibia.
Conclusion
This case report highlights the diagnostic and therapeutic challenges associated with multifocal, multicentric osteoid osteomas in 36-year-old male military personnel. The presence of lesions in both the tibiae and the skull, a rare occurrence, necessitated the use of comprehensive imaging techniques, including radiographs, CT scans, MRI, and bone scans, for accurate localization and diagnosis. Radiofrequency ablation (RFA) under CT guidance was successfully used to treat the multiple osteoid osteomas, demonstrating the efficacy of this minimally invasive technique. However, complications such as a second-degree burn at one ablation site, which requires further intervention, emphasize the need for meticulous procedural planning and vigilant postoperative care. This case underscores the importance of a multidisciplinary approach and thorough follow-up in managing multifocal osteoid osteomas. The discovery of an additional lesion in the frontal bone during follow-up highlights the necessity for ongoing vigilance. Future research should aim to refine diagnostic criteria and treatment protocols to improve patient outcomes and reduce complications.
References
1. Zhang Y, Rosenberg AE. Bone-forming tumors. Surgical pathology clinics. 2017 Sep 1;10(3):513-35.
2. Jaffe HL. Osteoid-osteoma: a benign osteoblastic tumor composed of osteoid and atypical bone. Archives of Surgery. 1935 Nov 1;31(5):709-28.
3. Kransdorf MJ, Stull MA, Gilkey FW, Moser Jr RP. Osteoid osteoma. Radiographics. 1991 Jul;11(4):671-96.
4. Ciftdemir M, Tuncel SA, Usta U. Atypical osteoid osteomas. European Journal of Orthopaedic Surgery & Traumatology. 2015 Jan;25:17-27.
5. Boscainos PJ, Cousins GR, Kulshreshtha R, Oliver TB, Papagelopoulos PJ. Osteoid osteoma. Orthopedics. 2013 Oct 1;36(10):792-800.
6. Touraine S, Emerich L, Bisseret D, Genah I, Parlier-Cuau C, Hamze B, et al. Is pain duration associated with morphologic changes of osteoid osteomas at CT? Radiology. 2014;271(3):795–804. doi: 10.1148/radiol.14131629.
7. Olvi LG, Lembo GM, Santini-Araujo E. Osteoid Osteoma. Tumors and Tumor-Like Lesions of Bone: Springer, London; 2015. p. 127–49.
8. Chai JW, Hong SH, Choi JY, Koh YH, Lee JW, Choi JA, Kang HS. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics. 2010 May;30(3):737-49.
9. Resnick D, Kyrriakos M, Greenway G. Tumors and tumor-like lesions of bone: imaging and pathology of specifc lesions. Bone and joint imaging. 3rd ed. Philadelphia: Saunders; 2005. p. 1120–30.
10. Kitsoulis P, Mantellos G, Vlychou M. Osteoid osteoma. Acta orthopaedica belgica. 2006 Apr 1;72(2):119.
11. Papathanassiou ZG, Panagiotis Megas MD, Theodore Petsas MD, Papachristou DJ, Nilas J, Dimitrios Siablis MD. Osteoid osteoma: diagnosis and treatment. Orthopedics (Online). 2008 Nov 1;31(11):1118.
12. Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. JBJS. 1992 Feb 1;74(2):179-85.
13. Goto T, Shinoda Y, Okuma T, Ogura K, Tsuda Y, Yamakawa K, Hozumi T. Administration of nonsteroidal anti-inflammatory drugs accelerates spontaneous healing of osteoid osteoma. Archives of orthopaedic and trauma surgery. 2011 May;131:619-25.
14. Laliotis NA, Bindoudi AS, Tsitouridis IA, Petrakis IG, Kirkos JM. Osteoid osteoma of the acetabulum: diagnosis and medical treatment. Journal of Pediatric Orthopaedics B. 2017 Nov 1;26(6):565-9.
15. Lindquester WS, Crowley J, Hawkins CM. Percutaneous thermal ablation for treatment of osteoid osteoma: a systematic review and analysis. Skeletal Radiology. 2020 Sep;49:1403-11.
16. Schai P, Friederich N, Krüger A, Jundt G, Herbe E, Buess P. Discrete synchronous multifocal osteoid osteoma of the humerus. Skeletal radiology. 1996 Oct;25:667-70.
17. Beck SE, Schwab JH, Rosenthal DI, Rosenberg AE, Grottkau BE. Metachronous osteoid osteoma of the tibia and the T7 vertebral body: a case report. JBJS. 2011 Jul 6;93(13):e73.
18. Scehajowicz F, Lemos C. Osteoid osteoma and osteoblastoma: closely related entities of osteoblastic derivation. Acta Orthopaedica Scandinavica. 1970 Jan 1;41(3):272-91.
19. de Ga K, Bateni C, Darrow M, McGahan J, Randall RL, Chen D. Polyostotic osteoid osteoma: A case report. Radiology case reports. 2020 Apr 1;15(4):411-5.
20. Aynaci O, Turgutoglu O, Kerimoglu S, Aydin H, Cobanoglu U. Osteoid osteoma with a multicentric nidus: a case report and review of the literature. Archives of Orthopaedic and Trauma Surgery. 2007 Dec;127:863-6.
21. Zmurko MG, Mott MP, Lucas DR, Hamre R, Miller PR. Multicentric osteoid osteoma. Orthopedics. 2004 Dec 1;27(12):1294-6.
22. Noordin S, Allana S, Hilal K, Nadeem N, Lakdawala R, Sadruddin A, Uddin N. Osteoid osteoma: contemporary management. Orthopedic reviews. 2018 Sep 9;10(3).
23. Kenan S, Abdelwahab IF, Klein MJ, Hermann G, Lewis MM (1994) Case report 864. Elliptical, multicentric periosteal osteoid osteoma. Skeletal Radiol 23:565–568
24. Allieu Y, Lussiez B, Benichou M, Cenac P (1989) A double nidus osteoid osteoma in a Wnger. J Hand Surg 14-A:538–541
25. Buluç L, Akansel G, Arslan A, Sarlak AY, Tosun B. Synchronous multicentric osteoid osteoma with associated fibrous cortical defect. Orthopedics (Online). 2008;31(1):95.
26. Garrigosa FL, Ledesma IG, Servat JJ. Large frontal osteoid osteoma with orbital extension. Orbit. 2013 Oct 1;32(5):336-7.
27. Nelson MC, Lack EE, Freedman MT. Multifocal osteoid osteoma in a 2.5 year-old child. Skeletal Radiol. 1994;23:465.
28. Rosenthal DI, Alexander A, Rosenberg AE, Springfield D. Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure. Radiology. 1992 Apr;183(1):29-33.
29. Motamedi D, Learch TJ, Ishimitsu DN, Motamedi K, Katz MD, Brien EW, Menendez L. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics. 2009 Nov;29(7):2127-41.
30. Lindner NJ, Ozaki T, Roedl R, Gosheger G, Winkelmann W, Wörtler K. Percutaneous radiofrequency ablation in osteoid osteoma. The Journal of Bone & Joint Surgery British Volume. 2001 Apr 1;83(3):391-6.
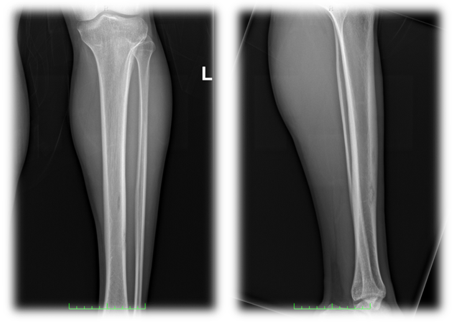
Figure 1
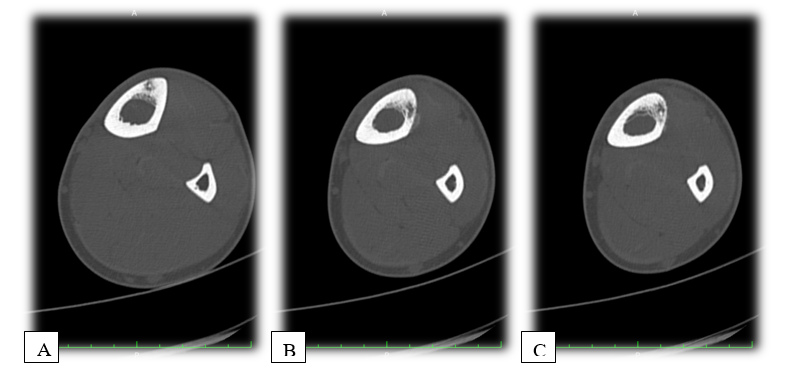
Figure 2
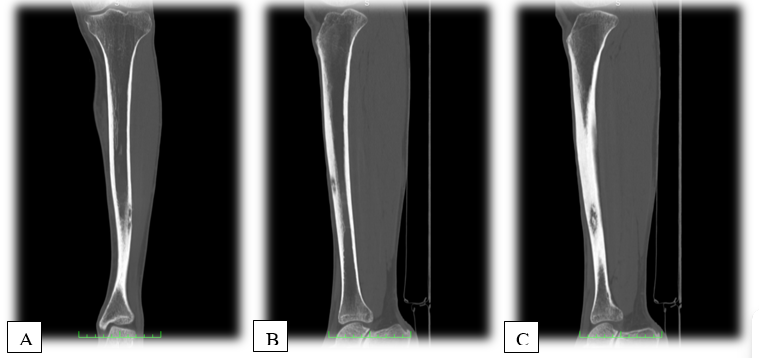
Figure 3

Figure 4
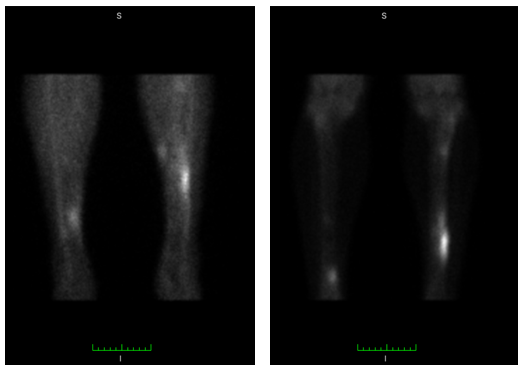
Figure 5
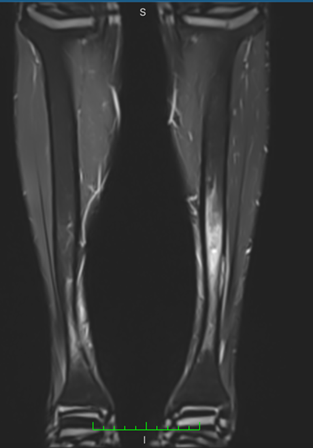
Figure 6
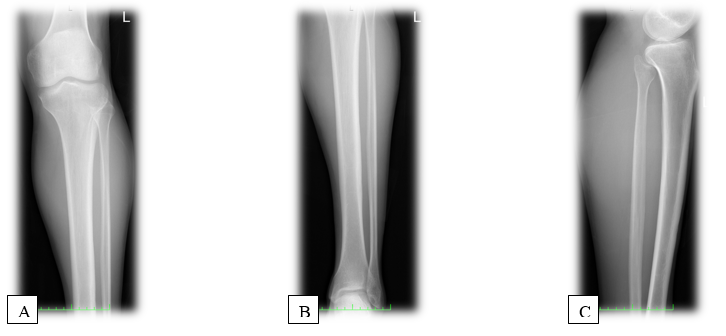
Figure 7

Figure 8
