Vulvovaginal Atrophy Treatment with PRP, Hyaluronic Acid, and Stem Cells in Postmenopausal Women
Vulvovaginal Atrophy Treatment with PRP, Hyaluronic Acid, and Stem Cells in Postmenopausal Women
Patricija Kasilovska*¹, Gianfranco Nicoletti ¹, Mario Goisis ², Riccardo Ossanna ³, Sheila Veronese ³,
Sara Ghazanfar Tehrani ³, Alessia Dallatana ³, Lindsey Alejandra Quinterosierra³, Chiara Curatola³,
Andrea Sbarbati ³, Zaneta Kasilovskiene 4
- University of Campania Luigi Vanvitelli, Naples Italy.
- DE Clinic, Milan Italy.
- University of Verona, Verona Italy.
- Medical Center Maxmeda, Vilnius Lithuania.
*Correspondence to: Patricija Kasilovska. University of Campania Luigi Vanvitelli, Naples Italy.
Copyright
© 2024 Patricija Kasilovska. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 04 September 2024
Published: 20 September 2024
DOI: https://doi.org/10.5281/zenodo.13821571
Abstract
To find out the characteristics of sexual life and factors influencing the health of postmenopausal women.
To achieve this goal, the following tasks have been formulated:
1. To analyze the peculiarities of sexual life and health disorders in the study group of women (45-60 years) who are menopausal and the distribution of symptoms.
2. To determine the influence of hormones on the sexual life of postmenopausal women.
3. To find out the most effective approaches to relieve menopausal symptoms and their distribution among patients.
4. To find out the influence of vulvovaginal atrophy and its treatment methods on a woman's sexual life.
Keywords: menopause, sexual dysfunction, female health, vulvovaginal atrophy, menopausal symptoms, stem cells, fat-derived products
Vulvovaginal Atrophy Treatment with PRP, Hyaluronic Acid, and Stem Cells in Postmenopausal Women
Abbreviations:
Abbreviations:
PRP- platelet rich plasma
HA- Hyaluronic acid
mesenchymal stem cells (MSCs)
adipose-derived MSCs (ADSCs)
IL-6 interleukin 6
IL-7 interleukin 7
Introduction
Menopause results from the cessation of ovarian follicle function and marks the end of menstruation. Clinically, menopause is diagnosed 12 months after the last menstrual period [2]. It occurs naturally, surgically, or medically. The number of middle-aged women is growing rapidly: in the 1990s, there were 467 million women aged 50 and over worldwide, and by 2030, the number of women of this age will increase to about 1200 million [2]. Most of the women experience menopause between the ages of 40 and 58, with an average age of 51 [6]. Due to the increasing life expectancy, approximately one-third of a woman's life is postmenopausal, which affects their health and quality of life [5].
Most of the women experience specific symptoms during menopause. Vasomotor symptoms, such as night sweats and hot flashes, are the only symptoms directly related to menopause [10, 11], occurring in 60–80% of women during menopause [12]. The majority of the women rate these symptoms as moderate to severe [13]. According to studies, most of the women have limited comprehension of menopause [17, 18]. By providing effective and reliable educational materials, menopausal women can be encouraged to prioritize their self-care and manage their symptoms [15].
Decreased estrogen level is associated with symptomatic vulvovaginal atrophy, a condition characterized by a thin, pale, and dry surface of the vagina and vulva. During menopause, the decline in estrogen levels leads to a decrease in lactobacilli, acid-producing bacteria that play a key role in maintaining the proper pH (3.8-4.5) of the vaginal epithelium [1]. As a result of decreasing in lactobacilli presence, the vaginal epithelium becomes more basal, which leads to changes in the vaginal flora. Moreover, increased bacterial diversity has been observed to correlate with increased symptoms of vaginal dryness [28]. In symptomatic vulvovaginal atrophy, there is often a decrease in secretion from the sebaceous glands, as well as a decrease in vaginal lubrication during sexual stimulation [1]. Women with vulvovaginal atrophy experience pain during intercourse, which reduces interest in intercourse and avoids it [30].
Sexual health is a crucial component of women’s well-being during menopause, but sexual life dysfunction tends to increase with age. Age-related decline in sexual function can significantly impair quality of life, so clinicians need to recognize sexual dysfunction to provide effective care for women during menopause. Moreover, sexual dysfunction can result from a variety of etiologies, including psychosocial factors, drug side effects, vulvovaginal atrophy, chronic disease, or hypoactive libido disorder. After finding out the aetiology and determining the factors that have a positive impact on sexual function, it will be possible to choose the proper treatment.
Sexuality affects the quality of life by affecting a woman's emotional and psychological health. The onset of menopause is a time characterized by hormonal, physiological, and social changes, often associated with sexual dysfunction. The physiological mechanism by which menopause affects sexual health is related to the decreasing and fluctuating levels of gonadal steroid hormones, which negatively affect the elasticity of the vaginal mucosa and the number of vaginal secretions, causing finally vaginal atrophy and pain during sexual intercourse [1]. As expectations for longer and healthier lives increase, women are thinking more about quality-of-life issues, including maintaining sexual function [3].
Women with partners who are more likely to engage in intimate sexual activity tend to be younger, have a lower body mass index, are married, and have better emotional well-being [33]. Despite a decrease in desire and arousal, many women still consider sex to be moderately or extremely important. During menopause, women with tertiary education have better physical and mental health outcomes, reflecting their overall quality of life compared to women with secondary education [3]. On the other hand, women with lower education levels often experience poorer mental health composites, emotional well-being, and social life [3], even if they do not report vaginal dryness as a distressing symptom. For women with symptomatic vulvovaginal atrophy, topical vaginal estrogen therapy is recommended [32]; low doses of vaginal estrogen are available in various forms like vaginal creams, pills, and rings. These low-dose treatments have minimal systemic absorption and are ineffective in relieving vasomotor symptoms [1]. Women who are receiving low-dose topical estrogen therapy should be carefully monitored for any uterine bleeding. For those who prefer not to use hormone therapy, over-the-counter water-based lubricants and moisturizers are available to help relieve symptoms.
There are currently no approved testosterone preparations for women to treat sexual dysfunction. Despite this, many medical providers still prescribe compounded testosterone or use testosterone products. The use of testosterone to treat female sexual function is controversial; serum-free and total testosterone levels are not related to the treatment of female sexual function [34].
In recent years, mesenchymal stem cells (MSCs) have acquired huge relevance for clinical applications because of their capacity to release many factors (such as hormones) and potential applications of regenerative medicine. Particularly, adipose-derived MSCs (ADSCs) have also been employed to secrete high quantities of cytokines and growth factors (fibroblast growth factor, keratinocyte growth factor, IL-6, and IL-7, among others) aimed at stimulating regenerative processes (18). ADSCs are highly present in the stromal vascular fraction of fat obtained following liposuction. They are reported in the literature to be effective for the treatment of different female sexual dysfunctions. A heterogeneous population characterizes the harvested fat and could promote revascularisation, activate local stem cell niches and modulate immune responses via the secretion of extracellular vesicles and hormones (16). Given the suitability to exploit fat tissue both for allogenic and autologous clinical applications, ADSCs have been extensively studied in the last years in order to exploit fat and fat-derived products without immune-inflammatory reactions (17). For these reasons, fat and its product represent an interesting potential treatment to apply to cure postmenopausal-related symptoms.
Notably, another treatment demonstrated to be effective for the cure of vulvovaginal atrophy is the regenerative medicine technique by the injection of platelet-rich plasma (PRP) or Dermgraft and Enriched Nanograft, a technique applied to process fat following liposuction. Platelet-enriched plasma and Enriched Nanograft therapy aim to stimulate the human body's self-healing capacity by increasing neovascularization and collagen formation due to high concentrations of autologous growth factors [50]. Dermgraft treatment aims to fill the loss of volume of the vulvar area, in particular, the labia majora.
The most significant advantages of this preparation are the possibility of using autologous material and the reliability [8, 9]. In the literature, there are different cases and studies on gynecological regenerative therapy [8, 9]. PRP and Nanofat have been used to treat atrophic conditions such as lichen sclerosus in the vagina, stress urinary incontinence, episiotomy scars, and lubrication disorders in the vagina [8]. This therapy was first used for the treatment of female sexual dysfunction by Charles Runels and named it "O-Shot" [9]. G-spot injection of PRP has been shown to improve sexual function.
Materials and Methods
The study was conducted at the Maxmeda medical institution and DE clinics in 2022 in January-May. It included postmenopausal women aged 45-60 years who agreed to participate, completed a questionnaire, and underwent a hormone test. Patients who agreed to participate in the study were interviewed using an anonymous questionnaire to find out the influence of their lifestyle and social factors on sexual behaviour and health disorders. Hormone tests were performed to assess estrogen, progesterone, and testosterone levels. The impact of lifestyle was assessed by answering the questionnaire about education, number of pregnancies, number of births, physical activity, smoking, alcohol consumption, and chronic diseases. Psychological, somatic, and vasomotor symptoms and sexual dysfunction were assessed using the Greene scale. Symptoms of sexual dysfunction were assessed in women who received hormone replacement therapy (HRT) and in those who did not use HRT. Vulvovaginal atrophy was assessed based on women's complaints and during gynecological examination. We divided women with vulvovaginal atrophy into four groups: Group 1 - patients treated with hyaluronic acid injection, Group 2 - patients treated with estrogen suppositories, Group 3 – patients treated with PRP method, and Group 4 - patients treated with adipose-derived stem cells (ADSCs), obtained with different mechanical fat manipulation method. We compared how each of the methods reduced the symptoms caused by vulvovaginal atrophy and the impact on sexual life. Standard computer programs MS Excel 2016 and SPSS 23.0 were used for statistical data analysis. Values calculated to be 95% were considered as reliable results. Differences were assessed as statistically significant when the confidence level was p <0.05. The results are presented in tables and diagrams.
Results
The study cohort comprised postmenopausal women aged 45-60. Two hundred four postmenopausal women completed the questionnaire. After analyzing the data collected during the survey on the social factors of the respondents, it was found that, according to our research, 50% have a higher / college education. We observed that the onset of symptoms influenced 85,1% of women. Between these, 12,7% did not give birth and were the ones with the more pronounced vasomotor and psychological symptoms. Overall, psychological symptoms occurred in 79,7% of women with symptoms, somatic symptoms in 39,8%, vasomotor symptoms in 60,6%, and sexual dysfunction in 47,3%. An association between menopausal duration and sexual dysfunction was observed (p <0,05), as was the case with lower estrogen levels. Smoking and alcohol consumption contributed to the onset of vasomotor and psychological symptoms. 30,3% of the respondents smoked and had a statistically significant increase in vasomotor and psychological symptoms (p <0,05). The research indicates the impact of alcohol consumption on quality of life and found that women who use alcohol had 73,4% more pronounced psychological symptoms. The results showed that almost half of the patients (47,3%) preferred hormone replacement therapy, 30,3% did not receive any treatment, and 37,7% preferred herbal preparations. Women with higher education prefer HRT; among these, 90% chose post-menstrual hormone therapy (PHT), while the usage of HRT was limited (18%). Assessing the distribution of symptoms of sexual dysfunction between women taking HRT and those not using it, it was found that women taking HRT had fewer symptoms of sexual dysfunction: 16,8% reported less sexual arousal. 81,6% who did not take hormone replacement therapy expressed having less sexual arousal, experiencing pain during intercourse, and orgasm disorders. The study included the relationship between the age of sexual partners and the perceived quality of sexual experiences in women. It indicated that women with younger ages (30-40 years) have better quality sex.
Vulvovaginal atrophy occurred in 52,6% of patients recruited for this study. The occurrence of vulvovaginal atrophy was observed to be affected by ingested estrogen levels, while testosterone levels did not affect vulvovaginal atrophy. Women with vulvovaginal atrophy were divided into three groups: 47 patients (47,4%) were treated with hyaluronic acid injection, 32 patients (32,3%) with estrogen vaginal suppositories, and the third group comprising 123 patients was treated with regenerative medicine methods; of the 123 patients 20,2% (n=20) were treated with platelet-rich plasma (PRP) and 50,9% (n=103) with stem cells. All patients complained of vaginal dryness, 78,7% of painful intercourse, and 49,4% of vaginal burning. We observed that injection of hyaluronic acid reduced vaginal dryness by 91,4%, estrogen suppositories by 78,1%, and PRP by 50%.
The adipose tissue was collected from 16 women undergoing liposuction to treat the vulvovaginal area, aged between 51 and 65. Informed consent was collected from every patient following the ethical guidelines established by the review committee for human studies of AOU “Ospedali Riuniti”, Ancona, Italy (Micro-adipose graft_01, 18 May 2017). The fat was harvested from the patients' flanks. 3 weeks before the harvesting, 6 sessions of acoustic wave therapy (AWT) were applied by the Duolith device (Storz, Switzerland) on the donor area of 8 of the 16 women. This treatment aimed to improve the regenerative power of the tissue. 120cc of Klein solution (2% Lidocaine solution: 0.08% w/v; Adrenaline 1mg/mL solution: 0,1% v/v in 0,9% saline) was injected 10 min before the liposuction. A cannula of 2 mm diameter, 6 holes (Go easy patented cannula), and a 60 mL Vac-Lock syringe (merit, USA) was used to obtain lipoaspirate (about 30 mL of fat from each donor). The fat was processed in Dermgraft (Go Easy system, Italy), Enriched Nanograft (Go Easy system, Italy), Micrograft (Lipocube, UK), Nanofat (Lipocube, UK), fat by Coleman technique, fluid fat by Seffigyn (Superficial Enhanced Fluid Fat Injection). The fat processed using the abovementioned techniques was transported in an adiabatic container to the laboratory and processed. The number of samples treated with each technique is as follows:
- 4 by Coleman technique
- 4 by Lipocube system/Micrograft
- 4 by Lipocube system/Nanofat
- 4 by Seffigyn (Superficial Enhanced Fluid Fat Injection)
- 4 by GOeasy.bio system (Dermgraft)
- 4 by GOeasy.bio system (enriched Nanograft)
Figure 1. Histological pictures of fat fragments obtained with different techniques: A) Coleman technique, B) GO easy. bio system (Dermgraft), C) Seffigyn (Superficial Enhanced Fluid Fat Injection), D) Lipocube system (Nanofat), E) Lipocube system (Micrograft), F) GOeasy.bio system (enriched Nanograft)
Figure 2. Cellular yield obtained with the different treatment: Coleman technique (A), GOeasy.bio system (enriched Nanograft) (B), Lipocube system (Nanofat) (C), Seffigyn (Superficial Enhanced Fluid Fat Injection) (D), GOeasy.bio system (Dermgraft) (E), Lipocube system (Micrograft) (F).
Figure 3. Cellular yield of patients treated with AWT compared to NOT AWT patients
Discussions
Many factors influence women's sexual activity: age, body mass index, marital status, sexual activity, place of residence, profession, social and economic environment, education, experienced sexual trauma and urogenital operations, psychological factors, and others. The partner's age, body mass index, profession and education also influence women's sexual activity [19].
A Chinese study showed that women aged 56–60 years had lower sex drive than women aged 45–55 years, and vaginal dryness and dyspareunia were more common in older study participants [20]. Age is believed to be an essential factor in women's sexual desire. It is also noteworthy that sexual dysfunction in middle-aged women was influenced by partner, alcohol consumption, vaginal dryness, dyspareunia, depressive symptoms and use of psychotropic drugs [21].
According to the data of a study conducted among Australian women (40-65 years old), 69,3% of respondents indicated a low sexual desire and identified factors related to it: vaginal dryness, pain during or after intercourse, moderate to severe depressive symptoms, and use of psychotropic drugs [22]. Looking at the world's research, in recent years, research on menopause and sexuality has mainly focused on the analysis of estrogen deficiency and its local or systemic replacement. However, androgens have recently returned to the spotlight as key regulators of female sexual health. It should be noted that preclinical and clinical studies consistently show that estrogens and androgens have a synergistic, stimulatory effect on women's sexual response, promoting sexual desire through a complex network of neurotransmitters and the balance between excitatory and inhibitory signals [23].
Vaginal atrophy is now included in the definition of a new term, orogenital menopause syndrome. This syndrome is also characterized by the following signs: vulvovaginal atrophy, urogenital atrophy or atrophic vaginitis. Most often, this syndrome is determined due to a decrease in estrogen levels in postmenopausal women or in women of any age who experience a reduction in estrogenic stimulation of the urogenital tissues. The signs and symptoms of vaginal atrophy are similar to many other genitourinary diseases, so the diagnosis, and therefore the treatment, is delayed. As a result of this disease, the anatomy and physiology of the urogenital system changes. Thus, an accurate diagnosis is essential, and hormonal or non-hormonal treatment can be applied [24]. The following are the most common signs of vaginal atrophy: pale, dry, smooth, shiny tissue, visible inflammatory changes (erythema, petechiae or increased visibility of blood vessels) [25].
HRT can be systemic (oral estrogens) or topical (intravaginal) estrogen, intravaginal estrogen release ring, and vaginal dehydroepiandrosterone (DHEA, testosterone)). Studies show that systemic HRT relieves symptoms in 75% of cases and local treatment in as much as 80-90% of cases. Side effects are similar, but topical treatment is safer than systemic treatment [26]. Symptoms and signs characteristic of vaginal arthrosis also appear in other vaginal diseases, making it more difficult for the doctor to make a proper diagnosis and choose treatment. During the differential diagnosis, it is necessary to exclude vulvovaginitis, including candidiasis, bacterial vaginosis, and trichomonosis. [27].
In 2017, one relevant case was analyzed during a different study, and in the author’s opinion, it is attractive for the final aim of the study. This case involved a 67-year-old woman who suffered from vaginal itching and irritation after menopause. She had these symptoms for five years and was treated with vaginal estrogen cream for more than a year. Despite long-term estrogen therapy, no significant clinical improvement in symptoms was observed. In addition to vaginal itching, the primary concerns were decreased volume of the labia majora and loss of tone. In order to restore the volume and contour of the labia majora, the woman was treated with lipophilic mixed with autologous PRP. Adverse outcomes were minimal; no short-term complications such as hematoma, lump or bump, or infection were observed. Lipophilization mixed with autologous PRP reduced clinical symptoms. One month after the injection, she was free of symptoms of vaginal itching and irritation that had persisted for more than five years before treatment. An increase in the volume of the labia majora was also evident after the operation. In addition, the lack of fullness and tone of the labia majora was corrected. Contour restoration was maintained well after one year. The white mottled lesions of lichen sclerosus around the labia minora also improved and did not recur [29].
Another exciting study to discuss in this context implies the treatment of 26 women affected by vulvovaginal atrophy (VVA) with monthly deep intradermal injections of hyaluronan. The patients were followed up six and twelve months after treatment. Dyspareunia during intercourse was the most common problem, but hyaluronic injections were effective in alleviating all gynecological symptoms. This treatment was safe and effective in helping women with VVA so that it could be offered as one of several treatments for VVA. Due to its pharmacodynamic properties and safety, hyaluronan could also be provided to women with oncological diseases who cannot take estrogenic drugs [31]. In this context, our study also showed that hyaluronic acid injection and PRP can be an alternative treatment for reducing the symptoms of vulvovaginal atrophy.
Regarding the derivation of fat-derived products, the analysis of the sample of the fat demonstrated that the enriched Nanograft (GOeasy.bio, Milan) is a new medical procedure that allows us to have a higher concentration of stem cells compared with other kits in the market (Lipocube, London - Seffiller, Bologna) because of selective filtration of the stromal vascular fraction. The cellular yield analysis confirms that the cell viability and yield are not affected by the manipulation technique but depend on the product-derived volume of treated adipose tissue. The clinical results on the patients showed that this represents a promising treatment for vulvovaginal atrophy. All the protocols applied in fat processing demonstrated clinical efficacy in the amelioration of vaginal symptomatology. The analysis of cell growth highlighted a significant difference in regenerative potential concerning the Enriched Nanograft, which showed higher cell growth. The regenerative capacity of the stem cells has been demonstrated to be evenly improved by the treatment of the donor area by AWT, albeit this treatment does not affect the cellular yield. To restore the volume of labia majora, the most helpful processing approach is represented by Dermgraft, which combines an excellent cellular reservation with a higher regenerative capacity of stem cells. Moreover, considering the cell growth ability, the improved cell growth ability was observed starting from 7 days of culture, suggesting that the technique influenced the stimulated growth. In particular, the cell growth statistically differed with Dermgraft and Enriched Nanograft.
Conclusions
1.Smoking and alcohol consumption influence the manifestation of vasomotor and psychological symptoms. The 57 patients who participated in the study reported that they smoked and had a statistically significant increase in vasomotor and psychological symptoms (p < 0.05). 138 female patients noted that they use alcohol and had more psychological symptoms. These symptoms were more pronounced in women who had not given birth.
2.The symptoms of sexual dysfunction were more pronounced in women whose menopause period was longer than five years.
3.When using hormone replacement therapy, the symptoms of sexual dysfunction appear less.
4.The use of hyaluronan injections, platelet-enriched blood plasma and stem cell treatment can be an alternative treatment method for vulvovaginal atrophy in women who do not want hormone treatment.
5.The age of the sexual partner affects the quality of sexual life. Women with younger partners (30-40 years old) have better sexual relations.
References
1. Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902. quiz 903–4. [PubMed] [Google Scholar].
2. A study on women’s health information needs in menopausal age BMC Womens Health. 2021; 21: 434. Published online 2021 Dec 28. doi: 10.1186/s12905-021-01582-0.
3. Hess R, et al. The impact of menopause on health-related quality of life: results from the STRIDE longitudinal study. Qual Life Res. 2012;21(3):535–44. [PMC free article] [PubMed] [Google Scholar].
4. Saei Ghare Naz M, Sayehmiri F, Kiani F, Ozgoli G: A Systematic Review and Meta-analysis on the Average Age of Menopause among Iranian Women J Evid Based Care 2019, 8(4):26–34.
5. El Khoudary SR, Greendale G, Crawford SL, Avis NE, Brooks MM, Thurston RC, Karvonen-Gutierrez C, Waetjen LE, Matthews K. The menopause transition and women's health at midlife: a progress report from the Study of Women's Health Across the Nation (SWAN) Menopause (New York, NY) 2019;26(10):1213–1227. [PMC free article] [PubMed] [Google Scholar].
6. The North American Menopause Society. The Menopause Guidebook. Menopause 101: A primer for the perimenopausal https://www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal.
7. Tian J, Cheng LH, Cui X, Lei XX, Tang JB, Cheng B. Application of standardized platelet-rich plasma in elderly patients with complex wounds. Wound Repair Regen. 2019; 27:268–76. [PubMed] [Google Scholar].
8. Neto JB. O-Shot: Platelet rich plasma in intimate female treatment. J Women’s Health Care. 2017; 6:395. [Google Scholar].
9. Runels C, Melnick H, Debourbon E, Roy L. A pilot study of the effect of localized injections of autologous platelet rich plasma (PRP) for the treatment of female sexual dysfunction. J Women’s Health Care. 2014; 3:3–6. [Google Scholar].
10. Santoro N, Roeca C, Peters BA, Neal-Perry G. The menopause transition: signs, symptoms, and management options. J Clin Endocrinol Metab. 2021;106(1):1–15. doi: 10.1210/clinem/dgaa764.[PubMed] [CrossRef] [Google Scholar].
11. Weidner K, Croy I, Siepmann T, Brähler E, Beutel M, Bittner A. Menopausal syndrome limited to hot flushes and sweating a representative survey study. J Psychosom Obstet Gynaecol. 2017;38(3):170–179. doi: 10.1080/0167482X.2017.1291624. [PubMed] [CrossRef] [Google Scholar]
12. Thurston RC, Joffe H. Vasomotor symptoms and menopause: findings from the Study of Women's Health across the Nation. Obstet Gynecol Clin North Am. 2011;38(3):489–501. doi: 10.1016/j.ogc.2011.05.006. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
13. Freeman EW, Sammel MD, Sanders RJ. Risk of long-term hot flashes after natural menopause: evidence from the Penn Ovarian Aging Study cohort. Menopause (New York, NY) 2014;21(9):924–932. doi: 10.1097/GME.0000000000000196. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
14. Puppo V. Anatomy and physiology of the clitoris, vestibular bulbs, and labia minora with a review of the female orgasm and the prevention of female sexual dysfunction. Clin Anat. 2013;26:134–52. [PubMed] [Google Scholar].
15. Du H-S, Ma J-J, Li M. High-quality Health Information Provision for Stroke Patients. Chin Med J (Engl) 2016; 129(17):2115–2122. doi: 10.4103/0366-6999.189065. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
16. American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. ACOG PRACTICE bulletin No. 119: Female sexual dysfunction. Obstet Gynecol. 2011;117:996–1007.[PubMed] [Google Scholar].
17. Gebretatyos H, Ghirmai L, Amanuel S, Gebreyohannes G, Tsighe Z, Tesfamariam EH. Effect of health education on knowledge and attitude of menopause among middle-age teachers. BMC Womens Health. 2020;20(1):232. doi: 10.1186/s12905-020-01095-2. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
18. Smail L, Jassim GA, Sharaf KI. Emirati Women's knowledge about the menopause and menopausal hormone therapy. Int J Environ Res Public Health. 2020;17(13):4875. doi: 10.3390/ijerph17134875. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
19. Moghasemi S, Ozgoli G, Ahmadi F, Simbar M. Sexual experience of Iranian women in their middle life: A qualitative approach. Int J Commun Based Nurs Midwifery. 2018;6(1):47–55. [PMC free article] [PubMed] [Google Scholar].
20. Zhang C, Cui L, Zhang L, et al. Sexual activity and function assessment in middle-aged Chinese women using the female sexual function index. Menopause. 2017;24(6):669–76. [PubMed].
21. Worsley R, Bell RJ, Gartoulla P, Davis SR. Prevalence and predictors of low sexual desire, sexually related personal distress, and hypoactive sexual desire dysfunction in a community-based sample of midlife women. J Sex Med. 2017;14(5):675–86.
22. Worsley R., Bell R.J., Gartoulla P., Davis S.R. Prevalence and predictors of low sexual desire, sexually related personal distress, and hypoactive sexual desire dysfunction in a community-based sample of midlife women. J. Sex. Med. 2017; 14:675–686. doi: 10.1016/j.jsxm.2017.03.254. [PubMed] [CrossRef] [Google Scholar].
23. Vignozzi L., Maseroli E. Hormones and sex behaviour. In: Petraglia F., Fauser B.C.J.M., editors. Endocrinology Female Reproductive Dysfunction. Springer; Berlin/Heidelberg, Germany: 2019. in press. [Google Scholar].
24. Faubion SS, Sood R, Kapoor E. Genitourinary Syndrome of Menopause: Management Strategies for the Clinician. Mayo Clin Proc. 2017 Dec;92(12):1842-1849.
25. Balica AC, Cooper AM, McKevitt MK, Schertz K, Wald-Spielman D, Egan S, Bachmann GA. Dyspareunia Related to GSM: Association of Total Vaginal Thickness via Transabdominal Ultrasound. J Sex Med. 2019 Dec;16(12):2038-2042.
26. Vaginal Atrophy Belal Bleibel; Hao Nguyen July 7, 2021.
27. Constantine G, Millheiser LS, Kaunitz AM, Parish SJ, Graham S, Bernick B, Mirkin S. Early onset of action with a 17β-estradiol, softgel, vaginal insert for treating vulvar and vaginal atrophy and moderate to severe dyspareunia. Menopause. 2019 Nov;26(11):1259–1264.
28. Hummelen R, et al. Vaginal microbiome and epithelial gene array in post-menopausal women with moderate to severe dryness. PLoS One. 2011;6(11):e26602. [PMC free article] [PubMed] [Google Scholar].
29. Seok Hwan Kim,1 Eun Soo Park, 1 and Tae Hee Kim2. Rejuvenation Using Platelet-rich Plasma and Lipofilling for Vaginal Atrophy and Lichen Sclerosus J Menopausal Med. 2017 Apr; 23(1): 63–68. Published online 2017 Apr 28. doi: 10.6118/jmm.2017.23.1.63.
30. Tan O, Bradshaw K, Carr BR. Management of vulvovaginal atrophy-related sexual dysfunction in postmenopausal women: an up-to-date review. Menopause. 2012;19(1):109–17. [PubMed] [Google Scholar].
31. Elisabetta Garavaglia,1 Cinzia Sala,2 Manuela Busato,1 Gilberto Bellia,3 Nadia Tamburlin,1 and Alberto Massirone1. First Use of Thermal Stabilized Hyaluronic Acid Injection in One-Year Follow-Up Patients with Genitourinary Syndrome. Published online 2020 Dec 4. doi: 10.2147/MDER.S275966.
32. North American Menopause, S. The 2012 hormone therapy position statement of: The North American Menopause Society. Menopause. 2012;19(3):257–71. [PMC free article] [PubMed] [Google Scholar].
33. Prairie BA, et al. A higher sense of purpose in life is associated with sexual enjoyment in midlife women. Menopause. 2011;18(8):839–44. [PMC free article] [PubMed] [Google Scholar].
34. Labia Majora Augmentation: A Systematic Review of the Literature. Jabbour S, Kechichian E, Hersant B, Levan P, El Hachem L, Noel W, Nasr M.Aesthet Surg J. 2017 Oct 16;37(10):1157-1164. doi: 10.1093/asj/sjx056.PMID: 28449124 Review.
35. esthet Surg J. 2021 Aug 13;41(9):1060-1067. doi: 10.1093/asj/sjaa118..
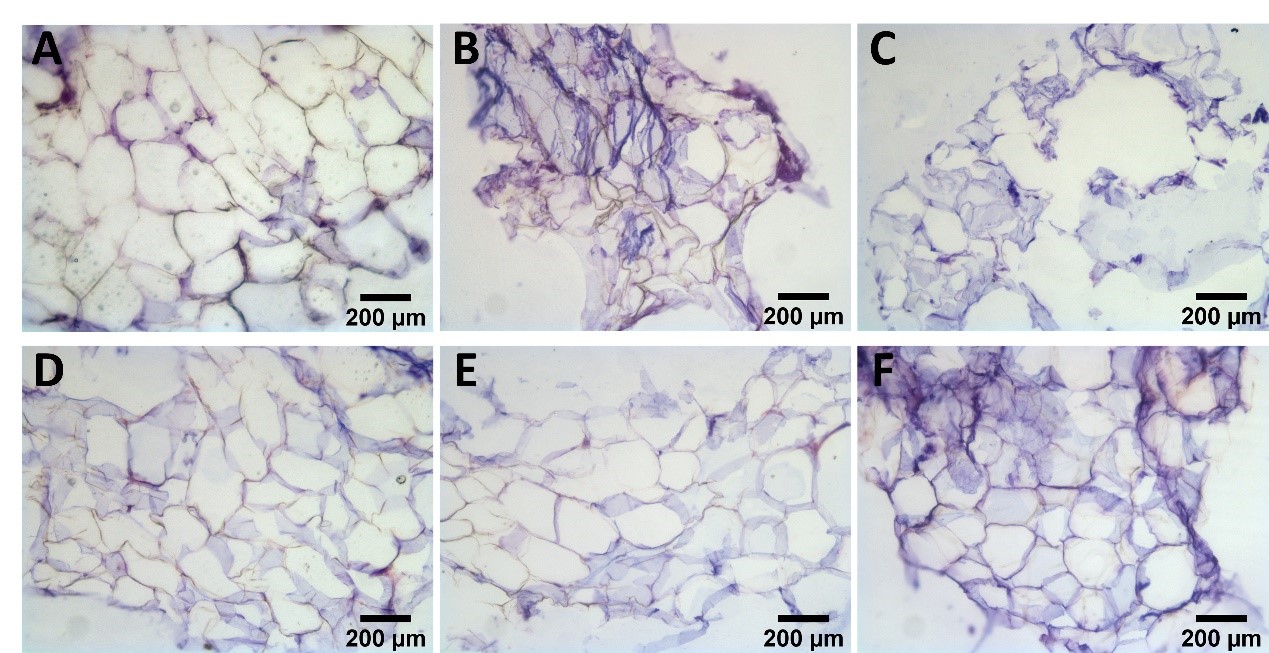
Figure 1
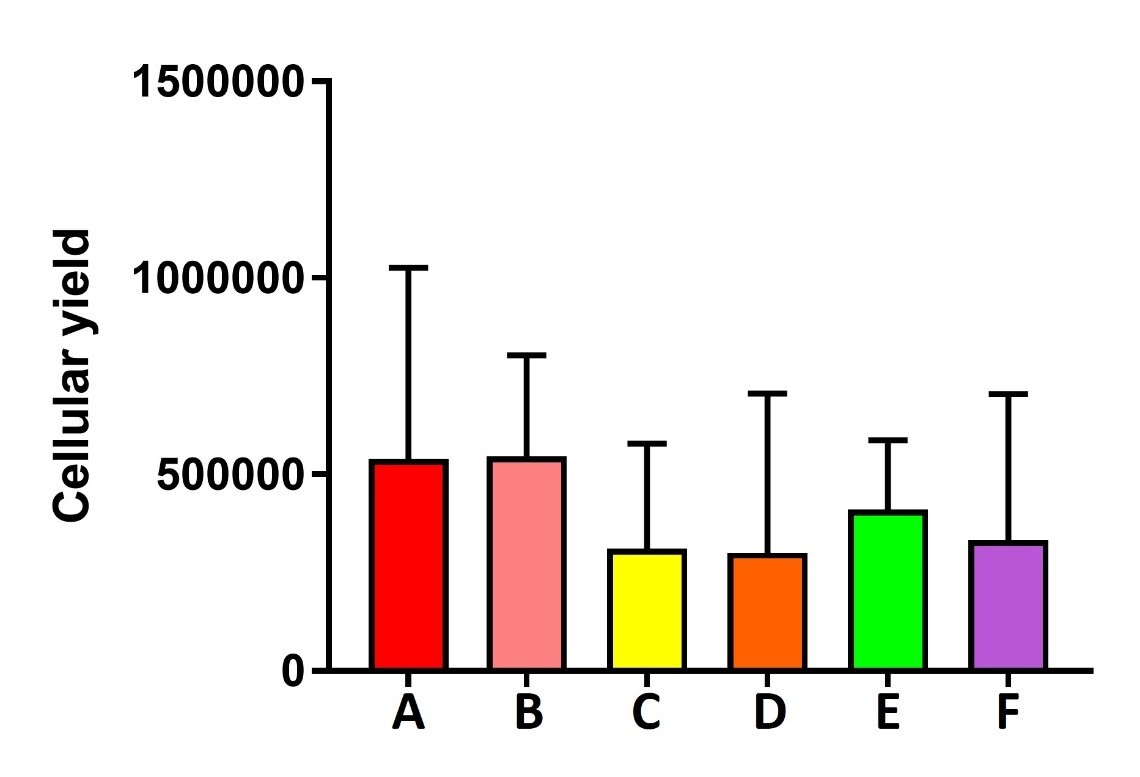
Figure 2
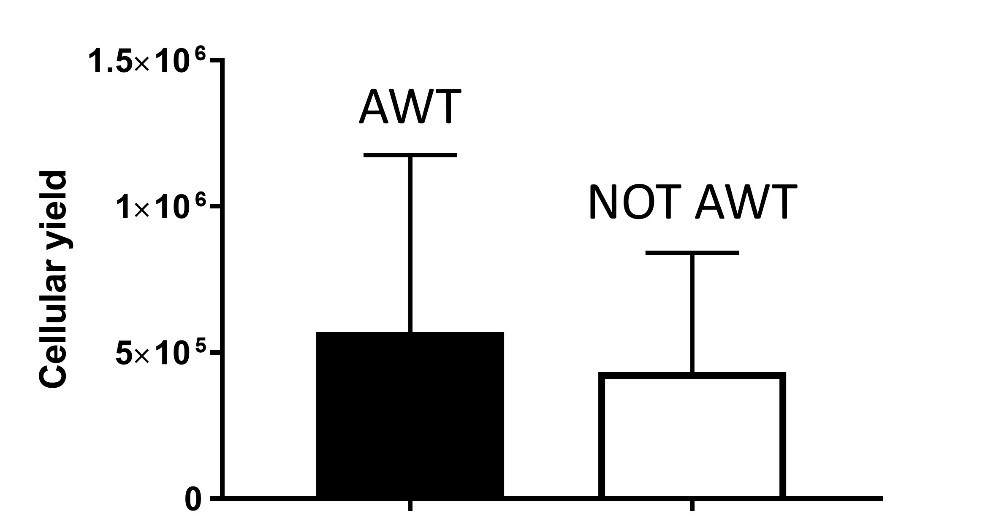
Figure 3
