Comparative Retrospective Research Examining the Effects of Anesthetic Type on Post-Hip Bipolar Hemiarthroplasty Mortality and Morbidity Case Study
Comparative Retrospective Research Examining the Effects of Anesthetic Type on Post-Hip Bipolar Hemiarthroplasty Mortality and Morbidity Case Study
Dr Sanjay Kumar Sureen *, Dr. Neeraj Bhardwaj1, Hasan Yousuf Bilal2
1. Dr. Neeraj Bhardwaj, Consultant Anesthesia, UK.
2. Hasan Yousuf Bilal, Prime Hospital, Dubai.
*Correspondence to: Dr Sanjay Kumar Sureen, Specialist Orthopedic Surgeon, prime hospital, Dubai, UAE.
Copyright
© 2024 Dr. Sanjay Kumar Sureen. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 21 Sep 2024
Published: 27 Oct 2024
DOI: https://doi.org/10.5281/zenodo.13892841
Abstract
Background: In the literature there are few studies that compare the effect of the type of anesthesia on mortality and morbidity after hip surgery. For hip fracture operations, besides the general anesthesia (GA) and neuro-axial block (NB) techniques, recently, the combined lumbar plexus and sciatic nerve block (CLSB) technique is recommended, especially for high-risk patients. The purpose of this study is to establish a relationship between the type of anesthesia and mortality and morbidity of hip fracture surgery.
Our hypothesis is that CLSB technique will decrease mortality and morbidity related to pulmonary and cardiovascular complications, thus reducing in-hospital stay of the patient and hospitalization cost.
Methods: we retrospectively reviewed the charts of 375 patients, who underwent hip hemiarthroplasty from year 2000 till year 2014, 213 patients underwent the surgery under CLSB anesthesia, 114 patients under general anesthesia, and 48 patients under neuro-axial block. Patients or their relatives were contacted for data collection about postoperative quality of life changes.
Results: one and five years survival rate was higher and possibility of perioperative complications was less after total hip hemiarthroplasty using CLSB anesthesia, time from trauma to operation was also a predictor for higher mortality. Patients who underwent operations under CLSB technique had better functional outcome at 3 month follow up.
Conclusions: To decrease the mortality rate after hip fracture and improve functional outcomes, since age and ASA status are patient-dependent factors that cannot be changed, patients must be operated on as soon as possible. Because CLSB is an encouraging technique to operate patients earlier, we recommend CLSB technique in hip fracture patients, especially for patients with poor general health status.
Comparative Retrospective Research Examining the Effects of Anesthetic Type on Post-Hip Bipolar Hemiarthroplasty Mortality and Morbidity Case Study
1. Introduction
Hip fractures are common injuries and almost always happen at old age and are caused by low velocity trauma, with the incidence of fracture rising dramatically after the age of 70 years. Patients with hip fractures are usually old, frequently troubled by multiple co-morbidities with more than 30% aged > 85 years [1]; economically these fractures constitute a large burden on healthcare [2].
Geriatric population with its multiple co-morbid conditions is at risk of developing anesthesia-related complications. Data on the impact of type of anesthesia on postoperative morbidity and mortality is limited. The effect of regional and general anesthesia on postoperative outcome needs to be clearly elucidated [4].
In the literature there are few studies that compare the effect of the type of anesthesia on mortality and morbidity after hip surgery with long term follow up especially after bipolar hemiarthroplasty.
For hip fracture operations, besides the general anesthesia (GA) and neuro-axial block (NB) techniques, recently, the combined lumbar plexus and sciatic nerve block (CLSB) technique is recommended, especially for high-risk patients [6–10].
When compared with GA and NB, the advantages of CLSB are minimal hemodynamic disturbance and so less affected cardio vascular stability [6–11].
NB is known to reduce mortality when compared with GA [5, 12, &13]; however, survival studies in hip fracture patients have not analyzed the e?ect of CLSB on mortality.
Previous observational studies have resulted in conflicting data regarding the association between anesthesia type and mortality after hip fracture surgery, no conclusion about the relationship between the anesthesia type choice and mortality [14]. In a recently published research about mortality after hip fracture [15], there was an uncertain relationship between mortality and anesthesia type.
Clinical trials comparing outcomes of regional versus general anesthesia for hip fracture offer insufficient insights to guide current practice because of exclusion of key patient groups, including those with delirium or dementia, [16, 17] and those undergoing hemiarthroplasty or total hip arthroplasty [18].
The purpose of this study is to establish a relationship between the type of anesthesia and mortality and morbidity of hip fracture surgery. Our hypothesis is that CLSB technique will decrease mortality and morbidity related to pulmonary and cardiovascular complications, thus reducing in-hospital stay of the patient and hospitalization cost.
2– Materials and Methods:
After obtaining the approval of the Research and Ethics Committee at multi centre study, a retrospective review of patients’ scanned medical records with detailed collection of data from charts of all the patients who underwent arthroplasty at our institution from 1st January 2000 till 31st January 2014 was done, 1034 charts were reviewed, 372 patient with elective hip surgery were excluded, 662 charts with the diagnosis of hip fracture were further studied, patients who underwent total hip replacement, patients with the diagnosis of Polytrauma on admission, patients with unknown type of anesthesia, and those who were lost in follow up were excluded from the study. Three hundred seventy-five (375) patients with history of traumatic hip fracture who underwent hip bipolar hermiarthroplasty were included.
The patients were divided into 3 groups according to anesthesia type as general anesthesia group (GA), neuro-axial block group (NB), and combined lumbar plexus and sciatic nerve block group (CLSB).
Anesthesia types were evaluated by anesthesia flow sheet.
Intraoperative period was divided into 4 time points:
- Base line – which is the time of induction of anesthesia.
- Incision time.
- Prosthesing – which is the time of insertion of the prosthesis.
- End time.
Data about intra-op vital signs monitoring i.e. blood pressure, heart rate, and pulse oxymeter; and medications given intra-op were collected according to these times.
We created indicator variables for the medications, which quantity was not recorded in the anesthesia flow sheet, as one if the medication was given and zero if it was not used; these medications were - Sevoflurane, N2O, and Levofed.
Gender, operated limb, age at admission, trauma date, drains, delay of operation, and duration of hospital stay were obtained from patients’ computerized scanned files of hospital charts, and folders.
Information about changes in mental status, post-op admission to critical care unit, in-hospital post-operative complications, blood transfusions, hemodynamic status was collected from patients’ daily progress notes.
All the patients were prescribed low-molecular-weight heparin for anticoagulation from admission to hospital to postoperative day 30, patients with impaired renal function received adjusted dose of anticoagulant.
Living patients or one of the relatives of the dead patients were interviewed by phone, changes in quality of life after surgery regarding activity status, estimated visual analogue pain score, the ability to self-service, limping, as well as the date of death for the passed-away patients were recorded.
The preoperative status of the patients was classified according to the American Society of Anesthesiologists (ASA) physical scale status to predict operative risk.
2.1Types of Anesthesia:
(1) GA: endotracheal anesthesia achieved by intravenous drugs (propofol and fentanyl), neuromuscular blockers (Cisatracurium besilate – Nimbex), and inhalation agents (Sevoflurane and N2O) to render the patient unconscious.
(2) NB – injection of local anesthetic agent bupivacaine 0.5% isobaric 2.5-3 mg/kg into the subarachnoid space was used.
(3) CLSB: posterior lumbar plexus block at paramedian levels for L2-L4 and posterior sciatic block done with 60 – 70 ml of the following mixture: (preparation per 20 ml):
(a) 5ml Xylocaine 2%.
(b) 4ml (1% Xylocaine +1/200.000 Adrenalin).
(c) 1cc Fentanyl l50 microgram.
(d) 10ml Bupivacaine isobaric 0.5%.
(e) ± Catapres 15 microgram.
2.2 Statistical Analysis.
The SPSS version 19.0 was used for data analysis, Chi – square and one way Anova were used to calculate frequencies (percent) and mean (standard deviation), the cumulative survival rates were obtained as Kaplan-Meier estimates, and the Breslow test was used to find P – value. To determine the association between potential predictors and mortality, Cox proportional hazards regression with multivariate analysis was used. P- value <0.05 was defined to be significant in all tests.
3– Results:
Three hundred seventy five patients met the inclusion criteria and were included in the study. There were three groups of patients according to anesthesia techniques: 114 patients with GA, 48 patients with NB, and 213 patients with CLSB. The baseline characteristics of the study population according to anesthesia techniques are summarized in Table 1.
Table1: Characteristics of the study population according to anesthesia type.
|
|
CLSB (n= 213) |
NB (n= 48) |
GA (n= 114) |
P-value |
|
Age Gender Male Female Operated limb Right hip Left hip Alzheimer Delay to operate |
78(8.96)
77(36.2%) 136(63.8%)
68(31.9%) 145(68.1%) 26(12.2%) 4.01(9.46) |
77.04(7.85)
21(43.8%) 27(56.3%)
23(47.9%) 25(52.1%) 8(17%) 3.75(5.84) |
70.75(13.51)
41(36%) 73(64%)
43(37.7%) 71(62.3%) 11(9.9%) 2.87(4.76) |
<0.0001
0.590
0.098 0.456 0.455 |
3.1 Demography:
There were no significant differences between the three groups regarding sex (P=0.590), operated side (P=0.098), preoperative mental status (P=0.456), and delay to operate (P=0.455). The patients’ mean age was 70.75 ±13.5 for GA, 77 ± 8 for NB, and 78 ± 9 for CLSB. Patients in GA group were significantly younger than in the other two groups. (Table1).
The ASA status among three groups was significantly different (P<0.0001). To compare the groups’ ASA status with each other, Mann-Whitney test was used. There was no significant difference in the ASA status between CLSB-NB (P=0.1), however, the ASA status was significantly different between CLSB and GA (P<0.0001) and GA and NB (P=0.032), CLSB patients’ health status was worse than the other groups. The ASA status of patients according to groups is shown thoroughly in Table 2.
Table2: ASA status of patients.
* P<0.05: CLSB patients’ ASA score is significantly worse than NB than GA patients.
|
ASA score
|
CLSB (n= 213) |
NB (n=48) |
GA (n=114) |
P-value |
|
1 2 3 4 |
0(0%) 13(6.1%) 162(76.1%) 38(17.8%) |
0(0%) 6(12.5%) 30(62.5%) 12(25%) |
4(3.5%) 36(31.6%) 51(44.7%) 23(20.2%) |
P<0.0001* |
|
Comparison of ASA - GA-NB |
P=0.030 |
|||
|
Comparison of ASA - GA-CLSB |
P<0.0001 |
|||
|
Comparison of ASA - NB-CLSB |
P=0.121 |
|||
3.2 Intraoperative data:
Regarding intra-operative data of monitored vital signs and hemodynamic stability and intra-operative complications, there was no significant difference between the groups regarding operative time (P=0.638), estimated blood loss (P=0.312), respiratory complications (P=0.679), heart rate at base (P=0.573) and prosthesing (P=0.381); pulse oximetry at the base (P=0.183) and mean arterial blood pressure at base (P=0.707) and incision time (P=0.392). (Table3).
Heart rate was significantly more stable during the incision time (P=0.034) and at the end of operations (P=0.014) in the CLSB group. (Table3).
The mean arterial blood pressure (MAP) was significantly more stable in the CLSB group during prosthesing and at the end of operation with P<0.0001 and P=0.045 respectively. (Table3).
There was significant difference in the necessity to keep hemovac in the operative wound and the use of Foley catheter with (P<0.002), the highest percentage of using hemovac was for patients in the GA group, while highest percentage of patients for whom Foley was inserted and for whom hemovac and Foley were used was in the NB group. (Table3).
Overall most of the patients were treated using cemented prosthesis P<0.0001, so was the majority of patients in the NB group 84%, compared to GA 51%, and CLSB 66%. (Table3).
Table3: Intra-operative data and complications
|
|
CLSB (n= 213) |
NB (n= 48) |
GA (n= 114) |
P-value |
|
Operative time(min)Drain None |
175.28(49.59) 59(27.7%) |
169.58(51.48) 6(12.5%) |
170.70(50.67) 18(15.8%) |
0.638 |
|
Foley |
4(1.9%) |
3(6.3%) |
0(0%) |
|
|
Hemovac |
137(64.3%) |
32(66.7%) |
90(78.9%) |
|
|
Hemovac and Foley |
13(6.1%) |
7(14.6%) |
6(5.3%) |
0.002 |
|
Heart rate/min |
|
|
|
|
|
Base |
82.23(10.17) |
83.69(12.48) |
83.33(12.25) |
0.573 |
|
Incision |
77.29(13.64) |
80(10.86) |
74.56(11.77) |
0.034 |
|
Prosthesing |
72.81(12.41) |
75.88(16) |
73.15(15.36) |
0.381 |
|
End |
75.74(11.73) |
81.15(10.68) |
78.2(14.16) |
0.014 |
|
Pulse oximetry |
|
|
|
|
|
Base |
99.29(2.67) |
98.92(2.63) |
99.61(0.98) |
0.183 |
|
Incision |
99.43(1.56) |
98.75(2.39) |
99.4(1.71) |
0.044 |
|
Prosthesing |
99.51(1.37) |
98.77(2.34) |
99.37(1.32) |
0.011 |
|
End |
99.56(1.39) |
99(1.95) |
99.44(0.99) |
0.041 |
|
Mean arterial pressure(MAP) |
|
|
|
|
|
Base |
95.9(12.53) |
94.4(11.35) |
95.28(10.84) |
0.707 |
|
Incision |
83.36(15.68) |
81.45(14.46) |
84.88(13.63) |
0.392 |
|
Prosthesing |
74.93(11.60) |
79.71(11.06) |
82.13(15.18) |
<0.0001 |
|
End |
86.66(12.41) |
86.39(7.92) |
89.73(9.61) |
0.045 |
|
Periprosthetic fracture |
0(0%) |
1(2.1%) |
0(0%) |
0.033 |
|
Kept on BYPAP |
1(0.5%) |
0 (0%) |
0(0%) |
0.679 |
3.3 Postoperative course in hospital:
Course of the patients postoperatively while in hospital is shown in Table 4. It includes data about admission to intensive care unit (ICU) or cardiac care unit (CCU) and its outcome, where there was no significance in the rate of admission to ICU/CCU between the groups (P=0.100), but the outcome of ICU/CCU was significantly different, most of the patients in the CLSB and NB groups recovered and were discharged from hospital, while all the patients of the GA group passed away while in the ICU/CCU.
No significant differences in some Post-operative complications were noted among the three groups such as supraventricular tachycardia (SVT) (P=0.215), unconsciousness (P=0.380), dyspnea (P=0.329), seizures (P=0.269), acidosis (P=0.215), hypoxia (P=0.225), pulmonary embolism (P=0.125), deep venous thrombosis (P=0.990), hallucination (P=0.615), wound infection (P=0.403), readmission within one month, and upper GI bleed (P=0.431). (Table4).
Patients with GA had more STEMI (P=0.031), pneumonia and atelectasis (P<0.0001), desaturation (P=0.014), constipation (P=0.021), confusion (P<0.0001), nausea, and vomiting (P<0.0001); while patients with NB had more urine retention (P=0.026), and agitation (P<0.0001). All the complications were less in the CLSB group. (Table4).
There was also significant difference in consumption of non-opioid analgesics postoperatively; patients with GA and NB used much more Paracetamol and Profenid than patients in the CLSB group (P<0.0001), while on the other hand, there was no difference in consumption of narcotics and opioids between the groups. (Table4).
Table4: Early post-operative data and complications (while patients still in hospital)
|
|
CLSB (n= 213) |
NB (n= 48) |
GA (n= 114) |
P-value |
|
Admission to ICU/CCU |
31(14.6%) |
7(14.6%) |
11(9.6%) |
0.431 |
|
Outcome of ICU/CCU Recovered |
|
|
|
|
|
27(90%) |
6(85.7%) |
0(0%) |
|
|
|
Seizure, unconscious |
2(6.7%) |
0(0%) |
0(0%) |
|
|
Passed away |
1(3.3%) |
1(14.3%) |
11(100%) |
<0.0001 |
|
STEMI |
0(0%) |
0(0%) |
3(2.6%) |
0.031 |
|
SVT |
4(1.9%) |
0(0%) |
0(0%) |
0.215 |
|
Unconsciousness |
3(1.4%) |
1(2.1%) |
0(0%) |
0.380 |
|
Pneumonia and Atelectasis |
43(20.2%) |
5(10.4%) |
43(37.7%) |
<0.0001 |
|
Dyspnea |
4(1.9%) |
1(2.1%) |
0(0%) |
0.329 |
|
Seizure |
8(3.6%) |
2(4.2%) |
2(1.8%) |
0.269 |
|
Desaturation |
7(3.3%) |
4(8.3%) |
13(11.4%) |
0.014 |
|
Acidosis |
4(1.9%) |
0(0%) |
0(0%) |
0.215 |
|
Hypoxia |
6(2.1%) |
0(0%) |
0(0%) |
0.225 |
|
Urine retention |
0(0%) |
2(4.2%) |
3(2.6%) |
0.026 |
|
Constipation |
0(0%) |
2(4.2%) |
3(2.6%) |
0.021 |
|
Upper GI bleed |
0(0%) |
0(0%) |
2(1.8%) |
0.100 |
|
PE |
7(3.3%) |
2(4.2%) |
0(0%) |
0.125 |
|
DVT |
4(1.9%) |
1(2.1%) |
2(1.8%) |
0.990 |
|
Wound infection |
10(4.7%) |
2(4.2%) |
2(1.8%) |
0.403 |
|
Alteration in mental status |
|
|
|
|
|
Hallucination |
4(1.9%) |
2(4.3%) |
3(2.7%) |
0.615 |
|
Agitation |
0(0%) |
6(12.8%) |
13(11.7%) |
<0.0001 |
|
Disorientation |
47(22.1%) |
6(12.8%) |
28(25.2%) |
0.221 |
|
Confusion |
9(4.2%) |
6(12.8%) |
26(23.4%) |
<0.0001 |
|
Nausea |
108(51.6%) |
25(53.3%) |
76(72.4%) |
<0.0001 |
|
Vomiting |
112(52.6%) |
28(58.3%) |
86(75.4%) |
<0.0001 |
|
Mean dosage of Paracetamol |
2.69(2.54) |
5.85(4.76) |
7.23(8.43) |
<0.0001 |
|
Mean dosage of Dolosal |
129.4(203.62) |
176.8(234.75) |
145.8(184.01) |
0.322 |
|
Mean dosage of Tramal |
1104(8682.9) |
435.63(542.2) |
214.04(266.9) |
0.474 |
|
Mean dosage of Profenid |
72.54(164.5) |
91.67(260.79) |
7.89(27.08) |
<0.0001 |
3.4 Patients’ progression at home:
Table 5 shows late post-operative data of patients’ progression at home, there was no difference in pain while moving where, mean visual analogue pain score was 1.54, 2.08, and 1.85 in the CLSB, NB, and GA groups respectively. There was no statistical difference in the percentage of patients who were able to walk at home, and those who used cane or crutches as ambulating aid, in the three groups.
The groups were comparable according to patients’ activities at home without any significant difference, although patients in CLSB performed better in means of putting shoes, and wearing socks 53.5% compared to 50% and 42.1% in the NB and GA groups respectively. (Table5).
Limping (P=0.081), dislocation rate (P=0.199), readmission within one month (P=0.262), and duration of hospital stay (P=0.158) were similar between groups. (Table5).
Pain at rest was least in the CLSB group, with mean visual analogue pain score of 0.77 compared to 1.23 in the other 2 groups. (Table5).
More patients in the GA group were bed ridden (P=0.032), where more patients from the CLSB group were able to climb stairs (P<0.0001), walk outdoor (P<0.0001), and use transport (P<0.001). (Table5).
Patients with CLSB could tolerate more time sitting in the chair in comparison with the other groups with P<0.0001. (Table5).
Table5: Late post-operative data of patients’ progression at home
|
|
Block (n= 213) |
Spinal (n= 48) |
General (n= 114) |
P-value |
|
Pain |
|
|
|
|
|
At rest |
0.77(1.14) |
1.23(1.51) |
1.23(1.98) |
0.028 |
|
While moving |
1.54(1.93) |
2.08(2.27) |
1.85(2.49) |
0.193 |
|
Walking ability |
|
|
|
|
|
Bed ridden |
51(23.9%) |
14(29.2%) |
43(37.7%) |
0.032 |
|
Within home |
155(72.8%) |
34(70.8%) |
67(58.8%) |
0.061 |
|
Climbing stairs |
111(52.1%) |
24(50%) |
31(27.2%) |
<0.0001 |
|
Walking outdoor |
89(41.8%) |
19(39.6%) |
22(19.3%) |
<0.0001 |
|
Using transport |
80(37.6%) |
16(33.3%) |
20(17.5%) |
0.001 |
|
Walking support |
|
|
|
|
|
Cane |
49(23%) |
11(22.9%) |
20(17.5%) |
0.496 |
|
Crutches |
0(0%) |
0(0%) |
2(1.8%) |
0.100 |
|
Walker None |
49(23%) 115(54%) |
9(18.8%) 28(58.3%) |
38(33.3%) 54(47.4%) |
0.063
|
|
Activities |
|
|
|
|
|
None |
70(32.9%) |
16(33.3%) |
48(42.1%) |
0.235 |
|
Putting shoes |
114(53.5%) |
24(50%) |
48(42.1%) |
0.144 |
|
Wearing socks |
114(53.5%) |
24(50%) |
48(42.1%) |
0.144 |
|
Self-service toilet usage |
139(65.3%) |
32(66.7%) |
60(52.6%) |
0.061 |
|
Limp |
55(25.8%) |
7(14.6%) |
19(16.7%) |
0.081 |
|
Chair sitting duration tolerability |
|
|
|
|
|
None |
36(16.9%) |
12(25%) |
36(31.6%) |
|
|
30 minutes |
50(23.5%) |
10(20.8%) |
39(34.2%) |
|
|
Hours |
127(59.6%) |
26(54.2%) |
39(34.2%) |
<0.0001 |
|
Dislocation |
6(2.8%) |
1(2.1%) |
0(0%) |
0.199 |
|
Hospital stay |
10.13(6.80) |
8.52(3.63) |
8.94(7.36) |
0.158 |
|
Readmission within one month |
5(2.3%) |
1(2.1%) |
0(0%) |
0.262 |
|
Alive |
133(62.4%) |
21(43.8%) |
48(42.1%) |
0.001 |
|
Time from operation to death (years) |
5.59(3.05) |
3.67(3.25) |
4.21(3.82) |
0.011 |
3.5 Mortality:
The one-year mortality rates of GA patients, NB patients, and CLSB patients were 41.7%, 35%, and 28.3%, respectively (P=0.034). One-year mortality rate was significantly lower in CLSB group than GA and NB groups. The overall mortality rates of GA patients, NB patients, and CLSB patients were 69.6%, 56%, and 33.7%, respectively (P<0.001). Overall mortality rate was significantly lower for CLSB than GA and NB groups. (Table6).
To determine the association between potential predictors of mortality (age, ASA status, delay to operate, operative time), Cox regression analysis was used. In the first Cox regression analysis GA was categorized as reference group, and NB and CLSB anesthesia types, were taken as variables in regards to the reference – CLSB group. Age (P<0.0001 ), delay to operate (P=0.056 ), operative time (P=0.008) and ASA (P=0.033) were found significant predictors of mortality. Both NB and CLSB choices combined were found to decrease mortality in this multivariate analysis (P=0.039). Since the anesthesia types were nominal variables in three different categories, we performed two more Cox regression analyses in order to find out the distinction between NB and CLSB choices. In the second Cox regression analysis, NB was not correlated with decreased mortality (P=0.65), when GA group was assigned as reference with regard to NB variable. However, in the third Cox regression analysis, GA and NB groups were collectively assigned as reference in regards to CLSB variable. CLSB was shown to decrease mortality significantly ( P<0.020, odds ratio = 0.471, confidence interval 0.250-0.889). Cox regression analyses are shown in Table7.
Estimated median survival time for CLSB patients was 6 years while, it was equal to 2 years for both NB and GA patients with 95% confidence interval of 4.93-7.06 for CLSB, 1.37-2.62 for NB, and 1.00-2.99 for GA. Estimated median survival time was significantly higher for CLSB than GA group and NB (P<0.001) Mortality rates are summarized in Table8, and survival curves are shown in Figure 1.
Table6 mortality rates between groups.
|
|
CLSB (n=213) |
NB(n=48) |
GA(n=114) |
P value |
|
One year mortality |
28.3% |
35% |
41.7% |
0.034 |
|
Overall mortality |
33.7% |
56% |
69.6% |
<0.001 |
Table7: Summary of Cox regression analyses.
|
|
P value |
Odds ratio |
95% confidence interval |
|
Age |
<0.0001 |
0.94 |
0.91-0.972 |
|
ASA score |
0.033* |
0.93 |
0.90-0.963 |
|
Delay to operate |
0.056* |
0.925 |
0.855-1.002 |
|
Operative time |
0.008* |
1.010 |
1.003-1.017 |
|
GA versus CLSB+NB (Cox 1) |
0.039* |
0.627** |
0.235-0.987 |
|
GA versus NB (Cox 2) |
0.65 |
1.021 |
1.042-1.055 |
|
GA+NB versus CLSB (Cox3) |
0.02* |
0.471** |
0.250-0.889 |
Table8: Estimated Survival analysis.
|
|
Estimated survival (years) |
95% Confidence Interval |
P-value* |
|
CLSB |
6 |
4.93-7.06 |
0.001 |
|
NB |
2 |
1.37-2.62 |
|
|
GA |
2 |
1.00-2.99 |
*Breslow
Figure1. The graph shows Kaplan-Meier survival curves for general anesthesia (GA), neuro-axial block (NB), and combined lumbar and sciatic block (CLSB) patients.
4– Discussion :
We retrospectively reviewed 375 patients with sub-capital hip fracture treated with bipolar hip hemiarthroplasty, operations were done under three types of anesthesia, the GA, NB, and the CLSB types, we tried to figure out the effect of the type of anesthesia on the mortality and morbidity and factors affecting patients’ progression postop in hospital and later on at home.
ASA physical scale status is commonly used to classify the preoperative status of the hip fracture patients [24-26]. Hamlet et al. [24] reported that 3-year mortality was significantly less for ASA I and II patients (23%) than for ASA III, IV, and V patients (39%). Michel et al. [25] reported that in 114 patients treated for hip fracture, high ASA status (III or IV) conferred a nine times increased risk for mortality at one year. However, in the review for anesthetic risk factors, Haljamäe [27] stated that because ASA classification considers only physical status factors, other risk-predictive factors such as age, gender, site of trauma, delay in surgical treatment, length of surgery, and the type of fracture pattern should also be included for individual cases; so we included patients who underwent only bipolar hemiarthroplasty after traumatic event so that we could unify the type and site of surgery and found that, age, delay to operate and length of surgery were also significant predictors of mortality.
These factors (age, delay in operation, and length of surgery) held a higher impact on survival when GA was used for patients with ASA III and IV. Our study also showed that patients who underwent the surgery under GA and who needed ICU or CCU later on in the hospital stay all passed away, this emphasizes more on the need to use other type of anesthesia in the critically ill patients of older age.
When the three groups of patients were compared, there were no significant differences in gender, operated side, mental status, and delay to operate. Similar to other studies [28, 29, and 30], delay to operate is associated with increased mortality in our study (P=0,028) (Table6).
Despite that the mean age of the GA patients was significantly younger than NB and CLSB patients, which would have decreased the mortality of GA patients as in other studies, [31-35], also, the ASA status of CLSB patients was significantly worse than GA and NB patients, that would have also increased the mortality of CSLB patients according to some studies [24-26], in our study the overall mortality rate was significantly less in the CLSB group, furthermore, the one year survival rate was better in the CLSB group so was the five year survival rate.
Sidi [36] showed that during the induction phase of GA Coronary vasospasm occurs, which leads to higher incidence of STEMI in patients at risk, our study also showed the same result with a significant P=0.031 value, thus it is advisable to sort patients according to ASA score and to avoid using GA to patients at high cardiac risk.
Atelectasis during GA is common, but usually does not cause clinically significant problems. Persistent prolonged atelectasis after GA increases perioperative respiratory complications. The use of N2O during GA renders patients to higher risk of developing atelectasis and subsequently pneumonia especially in obese patients with preexisting pulmonary comorbidities as shown by A. Hole [37]; our study showed that the use CLSB decreased the risk of developing these complications.
Papaioannou et. al [38] concluded that elderly patients subjected to GA display more frequent cognitive impairment during the immediate postoperative period in comparison to those who received a regional technique (NB or CLSB), the incidence of delirium was higher in patients with preexisting cardiovascular disease. In our study patients with GA had higher incidence of confusion in the early postoperative period. Patients with GA having higher probability of intra-operative atelectasis with preexisting cardiovascular disease should be anticipated to have some kind of decreased oxygen delivery to the brain which will affect their cognitive function and will be reflected as confusion as is the case in our study, especially if the patient receives a higher than needed dose of anesthetic agent during operation due to mismatch between estimated patient’s weight and real weight.
The use of volatile anesthetics is associated with a two-fold increase in the risk of post-operative nausea and vomiting (PONV), with risk increases in a dose-dependent manner, and no significant difference in incidence with different volatile anesthetics. In fact, the use of volatile anesthetics is the single most important factor for predicting emesis in the first 2 post-operative hours. [39] Nitrous oxide increases the relative risk of PONV by 1.4 times, opioid use increases the risk of PONV in a dose-dependent manner. Patients in our study who received GA had 2 fold incidence of having PONV while this risk was less with the other groups, the duration of operation and postop opioid consumption was statistically the same between groups which eliminates the effect of these variables on PONV and keeps the significant impact of the type of anesthesia.
In their study about Risk factors for urinary retention after hip or knee replacement, [40] Griesdale D., et al. concluded that Postoperative urinary retention is a common complication after total hip or total knee replacement, especially amongst men and patients receiving intrathecal morphine for anesthesia i.e. NB. Although we didn’t use morphine as anesthetic agent in our study, we also had increased risk of urinary retention after NB compared with GA and CLSB. Spinal agents influence the function of the lower urinary tract, by direct spinal action on the sacral nociceptive neurons and autonomic fibers, as well as by an effect on supraspinal centers. Urinary retention is less common after a short-acting (Lidocaine 5%) than after a long-acting agent (bupivacaine 0.5%) which we used for our patients for NB anesthesia and was found to decrease detrusor muscle strength and the ability to void. [41].
The one-year and overall mortality rates were decreased for the CLSB group. Also estimated survival time was higher for this group. In several studies, the reduction in morbidity and mortality had been shown with block anesthesia [28, 42]. In our study after eliminating patients’ individual data that would have affected mortality (age, sex, ASA, operated site, length of operation, and delay to operate) we found that CLSB choice was an independent variable of decreased mortality; and it had added protective value when used as anesthesia modality to high risk patients. Using the CLSB technique added to the survival of patients after bipolar hip hemiarthroplasty at least 3 years of life with 95% confidence interval (CI) 4.93-7.06 where patients who underwent the operation under GA or NB anesthesia had 1.00-2.99 CI.
Naja et al. [10] treated 60 patients for hip fracture, 30 patients with general anesthesia, and 30 patients with combined sciatic-paravertebral nerve block. They reported that both the incidence of intraoperative hypotension and the postoperative need for intensive care unit admission was significantly reduced in patients treated with combined sciatic-paravertebral nerve block compared to patients receiving general anesthesia. Similarly, in their prospective randomized study, de Visme et al. [6] treated 29 patients for hip fracture, 15 patients received combined lumbar and sacral plexus block, and 14 patients received spinal anesthesia. They found that hypotension was to be longer lasting after spinal anesthesia and of a larger magnitude in patients over 85 years of age. CLSB, as a rising trend, is correlated with minimal hemodynamic disturbance and so less affected cardiovascular stability [6–11]. These advantages of CLSB promote us to operate high-risk (ASA III AND IV) hip fracture patients earlier without seeking medical treatment modalities for their systemic diseases.
One of the withdraws of our study was the inability to evaluate patient’s BMI before operation, as all of the hip fracture patients are kept in complete bed rest regimen, formulas to estimate patient’s weight do exist but they are not accurate to use them in a study, and our facility is not equipped with built in weight measuring beds to obtain the needed data to study the effect of BMI on patient’s outcome and to precisely calculate the needed dose of anesthetic agents; as we think that obesity would affect patients’ overall performance and postop outcome, this should be a field to study in the future.
In conclusion, to decrease the mortality rate after hip fracture, since age and ASA status are patient-dependent factors that cannot be changed, the patients must be operated on as soon as possible. Because CLSB is an encouraging technique to operate patients earlier, we recommend CLSB technique in hip fracture patients, especially for patients with poor general health status and of old age. Considering the retrospective nature of the study, and the effects of personal characteristics, it is hard for us to claim that “CLSB technique decreases mortality.” Nevertheless, our hypothesis and results at least may form the basis and show the need for future randomized prospective studies.
However, the mean age of the GA patients was significantly younger than NB and CSLB patients, which would decrease the mortality of NB patients [31-35]. Also, the ASA status of CLSB patients was significantly worse than GA and NB patients that would increase the mortality of CLSB patients according to other studies [24-26].
References
[1] Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15,000 adults: the influence of age and gender. JBJS Br. 1998; 80:243-8.
[2] Hayes WC, Myers ER, Robinovitch SN, Van Den Kroonenberg A, Courtney AC, McMahon TA. Etiology and prevention of age-related hip fractures Bone. 1996 Jan; 18(1 Suppl.): 77S-86S.
[3] Parker MJ. The management of intracapsular fractures of the proximal femur. JBJS Br. 2000; 82:937-41.
[4] Rizwan Haroon Rashid, Hip Fracture Surgery: Does Type of Anesthesia Matter? Section of Orthopedics, Department of Surgery, Aga Khan University Hospital, Karachi 74800, Pakistan BioMed. Research International Volume 2013, Article ID 252356 (11 May 2013).
[5] M. J. Parker, H. H. Handoll, and R. Griths, “Anesthesia for hip fracture surgery in adults,” Cochrane Database of Systematic Reviews, no. 4, p. CD000521, 2004.
[6] V. de Visme, et Al., “Combined lumbar and sacral plexus block compared with plain bupivacaine spinal anesthesia for hip fractures in the elderly,” Regional Anesthesia and Pain Medicine, vol. 25, no. 2, pp. 158–162, 2000.
[7] N. Chia, T. C. Low, and K. H. Poon, “Peripheral nerve blocks for lower limb surgery—a choice anesthetic technique for patients with a recent myocardial infarction?” Singapore Medical Journal, vol. 43, no. 11, pp. 583–586, 2002.
[8] A. M. Ho and M. K. Karmakar, “Combined paravertebral lumbar plexus and parasacral sciatic nerve block for reduction of hip fracture in a patient with severe aortic stenosis, “Anesthesiology Research and Practice 5The Canadian Journal of Anesthesia, vol. 49, no. 9, pp. 946–950, 2002.
[9] Y. Asao, T. Higuchi, N. Tsubaki, and Y. Shimoda, “Combined paravertebral lumbar plexus and parasacral sciatic nerve block for reduction of hip fracture in four patients with severe heart failure,” The Japanese Journal of Anesthesiology,vol.54,no.6, pp. 648–652, 2005.
[10] Z.Naja, M.J.elHassan, H.Khatib, M.F.Ziade, and P.A.L¨ onnqvist, “Combined sciatic-paravertebral nerve block vs general anesthesia for fractured hip of the elderly,” MiddleEast journal of anesthesiology, vol. 15, no. 5, pp. 559–568, 2000.
[11] G. Fanelli, A. Casati, G. Aldegheri et al., “Cardiovascular effects of two di?erent regionalanesthetic techniques for unilateral leg surgery,” Acta Anaesthesiologica Scandinavica,vol.42, no. 1, pp. 80–84, 1998.
[12] L. A. Beaupre, C. A. Jones, L. D. Saunders, D. W. C. Johnston, J. Buckingham, and S. R.Majumdar, “Best practices for elderly hip fracture patients. A systematic overview of the evidence,”Journal of General Internal Medicine, vol. 20, no. 11, pp. 1019–1025, 2005.
[13] A. Rodgers, N. Walker, S. Schug et al., “Reduction of postoperative mortality and morbidity with epidural or spinal anesthesia: results from overview of randomized trials,” The British Medical Journal, vol. 321, no. 7275, pp. 1493–1497, 2000.
[14] O’Hara DA, Duff A, Berlin JA et al., The effect of anesthetic technique on postoperative outcomes in hip fracture repair.ANESTHESIOLOGY 2000; 92:947–57.
[15] H. Kesmezacar, E. Ayhan, M. C. Unlu, A. Seker, and S.Karaca, “Predictors of mortality in elderly patients with an intertrochanteric or a femoral neck fracture,” Journal ofTrauma, vol. 68, no. 1, pp. 153–158, 2010.
[16] Berggren D, Gustafson Y, Eriksson B, Bucht G, Hansson LI, Anesthesiology 2012; 117:72–92 Neuman et al. 79Reiz S, Winblad B: Postoperative confusion after anesthesia in elderly patients with femoral neck fractures. Anesth Analg 1987; 66:497–504.
[17] Valentin N, Lomholt B, Jensen JS, Hejgaard N, Kreiner S: Spinal or general anesthesia for surgery of the fractured hip? A prospective study of mortality in 578 patients. Br J Anaesth 1986; 58:284–91.
[18] Davis FM, McDermott E, Hickton C et al., Influence of spinal and general anesthesia on hemostasis during total hip arthroplasty. Br. J. Anaesth 1987; 59:561–71.
[19] Roche JJ, Wenn RT, Sahota O, Moran CG: Effect of comorbidities and postoperative complications on mortality afterhip fracture in elderly people: Prospective observational cohort study. BMJ 2005; 331:1374.
[20] Parker MJ, Handoll HH, Griffiths R: Anesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev 2004: CD000521.
[21] Glance LG, Osler TM, Mukamel DB, Dick AW: Impact of the present-on-admission indicator on hospital quality measurement: Experience with the Agency for Healthcare Research and Quality (AHRQ) Inpatient Quality Indicators. Med Care 2008; 46:112–9.
[22] Stukenborg GJ, Wagner DP, Harrell FE Jr et al., Hospital discharge abstract data on comorbidity improved the prediction of death among patients hospitalized with aspiration pneumonia. J Clin Epidemiol 2004; 57:522–32.
[23] Stukenborg GJ, Kilbridge KL, Wagner DP et al., Present-at-admission diagnoses improve mortality risk adjustment and allow more accurate assessment of the relationship between volume of lung cancer operations and mortality risk. Surgery 2005; 138:498–507.
[24] W. P. Hamlet, J. R. Lieberman, E. L. Freedman, F. J. Dorey, A. Fletcher, and E. E. Johnson, “Influence of health status and the timing of surgery on mortality in hip fracture patients,” American Journal of Orthopedics, vol. 26, no. 9, pp. 621–627, 1997.
[25] J. P. Michel, C. Klopfenstein, P. Hoffmeyer, R. Stern, and B. Grab, “Hip fracture surgery: is the pre-operative American Society of Anesthesiologists (ASA) score a predictor of functional outcome?” Aging—Clinical and Experimental Research, vol. 14, no. 5, pp. 389–394, 2002.
[26] V. Dzupa, J. Bartonícek, J. Skála-Rosenbaum, and V. Príkazský, “Mortality in patients with proximal femoral fractures during the first year after the injury,” Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca, vol. 69, pp. 39–44,2002.
[27] H. Haljamäe, “Anesthetic risk factors,” Acta chirurgica Scandinavica. Supplementum, vol. 550, pp. 11–9, discussion 19–21, 1989.
[28] L. A. Beaupre, C. A. Jones, L. D. Saunders, D. W. C. Johnston, J. Buckingham, and S. R. Majumdar, “Best practices for elderly hip fracture patients. A systematic overview of the evidence,” Journal of General Internal Medicine, vol. 20, no. 11,pp.1019–1025,2005.
[29] S. B. Sexson and J. T. Lehner Jr., “Factors affecting hip fracture mortality,” Journal of Orthopaedic Trauma, vol. 1, no. 4, pp. 298–305, 1987.
[30] P. Sircar, D. Godkar, S. Mahgerefteh, K. Chambers, S. Niranjan, and R. Cucco, “Morbidity and mortality among patients with hip fractures surgically repaired within and after 48 hours,” The American Journal of Therapeutics, vol. 14, no. 6,pp.508–513,2007.
[31] G. B. Aharonoff, K. J. Koval, M. L. Skovron, and J. D. Zuckerman, “Hip fractures in the elderly: predictors of one year mortality,” Journal of Orthopaedic Trauma, vol. 11, no. 3, pp. 162–165, 1997.
[32] H. M. Schroder and M. Erlandsen, “Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 2.5–18.5 years,” Journal of Orthopaedic Trauma, vol. 7, no. 6, pp. 525–531, 1993.
[33] J. A. Cipitria, M. M. Sosa, S. M. Pezzotto, R. C. Puche, and R. Bocanera, “Outcome of hip fractures among elderly subjects,” Medicina, vol. 57, no. 5, pp. 530–534, 1997.
[34] G. S. Keene, M. J. Parker, and G. A. Pryor, “Mortality and morbidity after hip fractures,” The British Medical Journal, vol. 307, no. 6914, pp. 1248–1250, 1993.
[35] A. Karagiannis, E. Papakitsou, K. Dretakis et al., “Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten-year follow-up with reference to the type of fracture,” Calcified Tissue International, vol. 78, no. 2, pp.72–77,2006.
[36] Sidi A, Dahleen L, Gaspardone A. “Coronary vasospasm during anesthesia induction: awareness, recognition, possible mechanisms, anesthetic factors, and treatment.”J.Clin.Anesth.2008Feb;20(1):64-9. doi:10.1016/j.jclinane.2007.02.016.
[37] A. Hole M.D.*, T. Terjesen and H. Breivik “Epidural Versus General Anaesthesia for Total Hip Arthroplasty in Elderly Patients” Article first published online: 30 DEC 2008 Acta Anaesthesiologica Scandinavica DOI: 10.1111/j.1399-6576.1980.tb01549.x.
[38] Papaioannou A1, Fraidakis O, Michaloudis D, Balalis C, Askitopoulou H. “The impact of the type of anaesthesia on cognitive status and delirium during the first postoperative days in elderly patients”. Eur J Anaesthesiol. 2005 Jul;22(7):492-9.
[39] Sébastien Pierre, MD, Rachel Whelan “Continuing Education in Anaesthesia, Critical Care & PainNausea and Vomiting After Surgery” Cont Edu Anaesth Crit Care and Pain. 2013;13(1):28-3. http://www.medscape.com/viewarticle/782388_3
[40] Griesdale DE, Neufeld J, Dhillon D, Joo J, Sandhu S, Swinton F, Choi PT. ”Can J Anaesth. 2011 Dec;58(12):1097-104. doi: 10.1007/s12630-011-9595-2. Epub 2011/Oct.
[41] Pertek JP1. Haberer JP. “Effects of anesthesia on postoperative micturition and urinary retention “, Ann Fr Anesth Reanim. 1995;14(4):340-51.
[42] A. Rodgers, N. Walker, S. Schug et al., “Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomized trials” The British Medical Journal, vol. 321, no. 7275, pp. 1493–1497, 2000
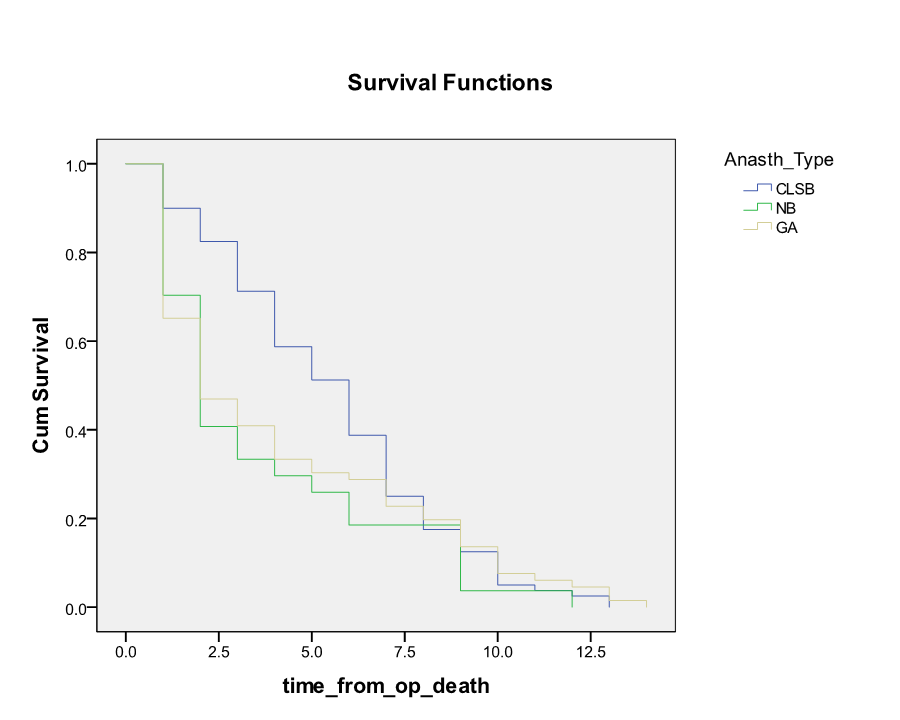
Figure 1
