An Analysis of 91 Patients with Minimum 2-Year Follow-Up Data Evaluating Paraspinal Muscle Approach for Neuromuscular Scoliosis and Perioperative Morbidity.
An Analysis of 91 Patients with Minimum 2-Year Follow-Up Data Evaluating Paraspinal Muscle Approach for Neuromuscular Scoliosis and Perioperative Morbidity.
Miodrag Milenkovic *
*Correspondence to: Miodrag Milenkovic, M.D, Orthopedic Surgeon, Czech Rehabilitation Hospital, UAE.
Copyright
© 2024 Miodrag Milenkovic. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 06 Sep 2024
Published: 01 Oct 2024
Abstract
The study focuses on the use of a paraspinal approach for neuromuscular scoliosis, focusing on deformity correction, perioperative morbidity, and outcome at a minimal follow-up length of 2 years. Data was collected from 61 patients operated using a paraspinal (Wiltse) approach between 2013 and 2019, and 104 control cases operated using a midline approach between 2005 and 2016. The results showed that Wiltse cases had comparable follow-up lengths, demographics, deformity corrections, complications, number of levels fused, and intensive care unit and hospital lengths of stay. Wiltse cases had lower estimated blood loss, allogenic transfusion rate, and operating time (ORT) than controls. However, only the number of levels fused and the ORT differed significantly according to the approach. The study concludes that the paraspinal approach for neuromuscular scoliosis is safe, associated with significant deformity correction, reduced estimated blood loss, and allogenic transfusion rate. Further evaluation of these benefits is needed, especially for cases with pelvic fixation.
Keywords: Paraspinal approach, midline incision, correction of deformity, perioperative morbidity, neuromuscular scoliosis.
An Analysis of 91 Patients with Minimum 2-Year Follow-Up Data Evaluating Paraspinal Muscle Approach for Neuromuscular Scoliosis and Perioperative Morbidity.
Introduction
The posterior paraspinal muscle approach, similar to the Wiltse approach, is commonly used for spinal trauma, degenerative, and neoplastic adult cases, and is increasingly being used for adult spine deformity. It offers potential advantages over the posterior midline approach, such as reduced soft tissue trauma, lower post-operative pain, opioid consumption, estimated blood loss (EBL), allogenic transfusion rate, and length of stay (LOS). The best evidence supporting these advantages has been shown for adolescent idiopathic scoliosis (AIS) patients. A large retrospective comparative study comparing 192 cases operated using a paraspinal muscle approach to 293 cases operated through a midline approach showed a lower opioid consumption, EBL, and transfusion rate, and a shorter hospital LOS for the paraspinal muscle group. However, literature reporting the use of this approach for neuromuscular scoliosis (NMS) is scarce. This study aimed to compare the deformity correction, intraoperative parameters, and safety of the posterior paraspinal muscle approach (Wiltse) to the use of the posterior midline approach for treating NMS patients. The primary hypothesis was that the Wiltse approach allows comparable deformity correction, lower intraoperative and perioperative complication rates, lower EBL, and hospital LOS.
Materials and Methods
The Wiltse approach, a surgical technique used in neuromuscular syndrome (NMS) patients, has been used by three senior surgeons since August 2013. A total of 61 NMS patients were operated between August 2013 and June 2019 using this approach, and an additional series of 104 control patients were included. The control patients were operated by two senior surgeons at two tertiary institutions using a posterior midline approach between November 2005 and March 2016. The Wiltse and control patients with a clear neuromuscular pathology leading to NMS were retrospectively compared.
The collected data included age, gender, body mass index (BMI), the diagnosis leading to NMS, the pre-operative gastrostomy tube and/or respiratory assistance presence, major curve, and pelvic obliquity measurements. Complications were recorded and categorized in function of their chronological occurrence in relation to the timing of the surgery. Perioperative complications were reported globally, independently of their origin, and as approach-related complications.
The surgical variables were assessed globally and with subgroup analysis according to the presence or absence of pelvic fixation: number of levels fused, operating time (ORT), EBL, percentage of EBL of estimated blood volume, allogenic transfusion rate, and the ICU and hospital LOS. The ORT was calculated from the time of incision to the wound closure. The anesthetic team evaluated the EBL by counting blood loss in the suction cannula and cell saver. Surgical sponges were not typically used, but if used, they were also taken into account for blood loss estimation. The estimated blood volume was calculated as 70mL/kg (weight). Tranexamic acid and cell saver were used for all cases, and a uniform post-operative protocol was followed.
The surgical technique used was a single midline skin incision extending from upper to lower instrumented vertebra and following the spinous processes. No fluoroscopy was used to determine the length and localization of it. After skin incision, the skin was undermined laterally to allow paramedian extraperiosteal bilateral fascial incisions. A blunt, muscle-sparing approach was used down to the facet joints in the lumbar spine, respectively, to the transverse processes in the thoracic spine. If pelvic fixation was performed, the skin was more laterally undermined in the caudal aspect of the incision up to the posterior superior iliac spine (PSIS). The cortex was opened at the PSIS with a Luer to avoid screw head protrusion and the Iliac bone was cannulated using free-hand technique. Wide facetectomies were performed, and the pedicles were cannulated using a free-hand technique.
After the exposure, facetectomies, pedicle marker introduction, decortication, and bone grafting were performed on both sides, and definitive instrumentation was undertaken. Cannulated pedicle screws connected to reduction tubes were inserted on the convex or concave side of the major curve, as was the surgeon’s preference. After all the pedicle screws were introduced, two 5.5-mm diameter cobalt-chrome rods were cut to the measured length. Rod de-rotation or translation with gradual spine-to-rod reduction was used to correct most of the deformity. In case of pelvic fixation, each rod was connected to the ipsilateral iliac screw using a transverse connector which was transmuscularly tunneled.
The study had institutional ethical approval (CCER 15152). The Shapiro–Wilk test was used to evaluate the data distribution’s normality, and the characteristics depicting normal distribution between groups were compared using unpaired Student’s t-tests and Pearson’s chi-square test for dichotomous outcomes. The initial major curve correction was significant, even when significance was set at p<0.0001, and equivalent in both groups (Wiltse 39° or 57%, controls 44° or 60%, p-values=0.153 and 0.421) and lasted at final FU (Wiltse 39° or 57%, controls 42° or 56%, p-values=0.440 and 0.817). The initial pelvic obliquity correction was 6° in both groups (p-value=0.668) and remained 6° at final FU (p-value=0.938).
Table 1: Baseline parameters, including diagnosis leading to NMS.
Table 2: Surgical variables and approach-related perioperative complications by group, with additional subgroup comparison (with vs without pelvic fixation).
Table 3: Complications (intraoperative; perioperative (≤30 days) (global vs approach-related); late post-operative (>30 days)) and mortality.
Discussion
The study aimed to compare the complication rates of Wiltse and control patients with non-mandibular spondylitis (NMS) surgery. Both groups achieved similar mean initial and final post-operative major curve and pelvic obliquity corrections, with no significant differences in mortality rate, intraoperative, perioperative (global and approach-related), and late complication rates between the two groups. Wiltse cases had lower EBL, percentage of EBL of estimated blood volume, and allogenic transfusion rate when considering all patients, selectively the cases without pelvic fixation.
The mean initial major curve correction of Wiltse and control patients was equivalent for both groups, lasted at final FU, and fell within the range of correction reported in the literature for NMS patients using all pedicle screw constructs and a posterior midline approach. Both groups achieved an equivalent initial pelvic obliquity correction, which persisted at final FU and was comparable to the mean pelvic obliquity correction of 56% or 5.2° reported by Modi et al., using a posterior midline approach.
The intraoperative complication rate was similar for both approaches, but more serious complications occurred in the posterior midline approach group. This finding cannot be attributed to variations in tranexamic acid use or nutritional status, as tranexamic acid was always used. The mean BMI, pre-operative gastrostomy tube presence rate, and pre-operative gastrostomy tube presence were comparable in both groups.
Mortality rate, perioperative, and late complication rates were not significantly different in Wiltse cases compared to Controls. However, Wiltse cases had tendentially less complications of this type than Controls. The study found that surgery-related complications result from increased blood loss, longer ORT, and extensive tissue dissection due to curve severity and pelvic fixation.
Previous studies have reported high perioperative complication rates for NMS surgeries, with some disease-related factors influencing the complication rates. The study found a complication rate of 0% for Wiltse and 4% for control patients using the "SRS M&M" database.
Wiltse patients experienced less EBL (535 vs 1187 mL) and lower allogenic transfusion rates (48% vs 96%) than controls considering all patients, and when selecting those without pelvic fixation (n = 71 among 91). No statistical differences of EBL or transfusion rates were found according to the used approach. The Wiltse group globally had less EBL and lower transfusion rates despite holding a higher proportion of patients with pelvic fixation than the control group do (30% vs 13%).
Edler et al. found that neuromuscular patients had an almost seven times higher risk of losing >50% of their estimated total blood volume during scoliosis surgery. Modi et al. reported a mean EBL of 3221 mL when performing standard PSF in NMS cases. McLeod et al. retrospectively reviewed the "Pediatric Health Information Systems" database between 1 January 2006 and 30 September 2009, analyzing 2722 AIS and 1547 NMS procedures for antifibrinolytics use and blood transfusions in US children's hospitals. They reported the median hospital-specific rate of red cell transfusions in NMS was 43% for NMS and 24% for AIS. In NMS, antifibrinolytics use did not decrease the odds of transfusions.
Kieser et al. reported a mean EBL of 2439 mL versus 795 mL in their retrospective series comparing 8 NMS patients operated using the posterior midline approach with 16 NMS patients operated using a paraspinal muscle approach. This statement is consistent with several publications comparing both approaches for AIS correction which found an association between the paraspinal approach use and decreased EBL and transfusion rate. Possible explanations for the reduced EBL and transfusion rates observed when using the paraspinal muscle approach might be that it is an anatomic approach taking advantage of avascular intermuscular planes and reduced exposed bone area using subperiosteal dissection.
The study compared the ICU LOS of Wiltse and control cases, with a LOS of 6 versus 5 days for Wiltse patients and 4.7 days for control cases. The hospital LOS was globally equivalent for both approaches, with a 9.2 versus 10.3 days average hospital LOS for NMS children. The hospital LOS was significantly shorter in Wiltse patients compared to control patients, with a shorter LOS for Wiltse cases. This was also reported in a retrospective study comparing AIS cases operated using a Wiltse or a posterior midline approach. However, the study has limitations, such as a retrospective design, exclusion of control cases due to lack of functional outcome data, and a larger time frame compared to Wiltse patients. Despite these, the study has strengths, including the first report with a minimal functional outcome of 2 years and comprehensively reported baseline parameters.
Conclusion
The study suggests that paraspinal muscle approach (Wiltse) for non-muscular system (NMS) patients can provide effective initial and long-lasting deformity correction, potentially being safer due to no surgery-related complications. Wiltse is associated with reduced early bone loss (EBL), lower allogenic transfusion rate, and shorter hospital stay in the subgroup without pelvic fixation. Further evaluation of these benefits is needed with larger cohorts.
References
1. Uddin OM, Haque R, Sugrue PA, et al. Cost minimization in treatment of adult degenerative scoliosis. J Neurosurg Spine 2015; 23(6): 798–806.
2. Uribe JS, Beckman J, Mummaneni PV, et al. Does MIS surgery allow for shorter constructs in the surgical treatment of adult spinal deformity? Neurosurgery 2017; 80: 489–497.
3. Anand N, Baron EM, Khandehroo B, et al. Long-term 2-to 5-year clinical and functional outcomes of minimally invasive surgery for adult scoliosis. Spine 2013; 38: 1566–1575.
4. Anand N, Baron EM, Thaiyananthan G, et al. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech 2008; 21(7): 459–467.
5. Anand N, Rosemann R, Khalsa B, et al. Mid-term to longterm clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus 2010; 28(3): E6.
6. Yen CP, Mosley YI and Uribe JS. Role of minimally invasive surgery for adult spinal deformity in preventing complications. Curr Rev Musculoskelet Med 2016; 9(3): 309–315 . Sarwahi V, Galina JM, Hasan S, et al. Minimally invasive versus standard surgery in idiopathic scoliosis patients: a comparative study. Spine 2021; 46: 1326–1335.
8. De Bodman C, Miyanji F, Borner B, et al. Minimally invasive surgery for adolescent idiopathic scoliosis: correction of deformity and peri-operative morbidity in 70 consecutive patients. Bone Joint J 2017; 99-B(12): 1651–1657.
9. Miyanji F, Samdani AF, Ghag A, et al. Minimally invasive surgery for AIS: an early prospective comparison with standard open posterior surgery. J Spine 2013; 5: 1–4.
10. Sarwahi V, Horn JJ, Kulkarni PM, et al. Minimally invasive surgery in patients with adolescent idiopathic scoliosis. Clin Spine Surg 2016; 29: 331–340.
11. Sarwahi V, Amaral T, Wendolowski S, et al. Minimally invasive scoliosis surgery: a novel technique in patients with neuromuscular scoliosis. Biomed Res Int 2015; 2015: 481945.
12. Kieser DC, Thakar C, Cunningham G, et al. The value of a modified wiltse approach for deformity correction in neuromuscular scoliosis. Int J Spine Surg 2020; 14(2): 170–174.
13. Feldman JM, Roth JV and Bjoraker DG. Maximum blood savings by acute normovolemic hemodilution. Anesth Analg 1995; 80(1): 108–113.
14. Sarwahi V, Wollowick AL, Sugarman EP, et al. Minimally invasive scoliosis surgery: an innovative technique in patients with adolescent idiopathic scoliosis. Scoliosis 2011; 6: 16.
15. Wiltse LL, Bateman JG, Hutchinson RH, et al. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 1968; 50: 919–926.
16. Kim YJ, Lenke LG, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe. Spine 2004; 29: 333–342.
17. Toll BJ, Samdani AF, Janjua MB, et al. Perioperative complications and risk factors in neuromuscular scoliosis surgery. J Neurosurg Pediatr 2018; 22(2): 207–213.
18. Modi HN, Hong J-Y, Mehta SS, et al. Surgical correction and fusion using posterior-only pedicle screw construct for neuropathic scoliosis in patients with cerebral palsy: a threeyear follow-up study. Spine 2009; 34: 1167–1175.
19. Heffernan MJ, Seehausen DA, Andras LM, et al. Comparison of outcomes after posterior spinal fusion for adolescent idiopathic and neuromuscular scoliosis: does the surgical first assistant’s level of training matter? Spine 2014; 39: 648–655.
20. Tsirikos AI and Mains E. Surgical correction of spinal deformity in patients with cerebral palsy using pedicle screw instrumentation. J Spinal Disord Tech 2012; 25(7): 401–408.
21. Rumalla K, Yarbrough CK, Pugely AJ, et al. Spinal fusion for pediatric neuromuscular scoliosis: national trends, complications, and in-hospital outcomes. J Neurosurg Spine 2016; 25(4): 500–508.
22. Mohamad F, Parent S, Pawelek J, et al. Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 2007; 27(4): 392–397.
23. Cognetti D, Keeny HM, Samdani AF, et al. Neuromuscular scoliosis complication rates from 2004 to 2015: a report from the Scoliosis Research Society Morbidity and Mortality
database. Neurosurg Focus 2017; 43: E10.
24. Edler A, Murray DJ and Forbes RB. Blood loss during posterior spinal fusion surgery in patients with neuromuscular disease: is there an increased risk? Paediatr Anaesth 2013; 13: 818–822.
25. Modi HN, Suh S-W, Yang J-H, et al. Surgical complications in neuromuscular scoliosis operated with posterior- only approach using pedicle screw fixation. Scoliosis 2009; 4: 11.
26. McLeod LM, French B, Flynn JM, et al. Antifibrinolytic use and blood transfusions in pediatric scoliosis surgeries performed at US Children’s Hospitals. J Spinal Disord Tech 2015; 28(8): E460–E466.
27. Miyanji F and Desai S. Minimally invasive surgical options for adolescent idiopathic scoliosis. Semin Spine Surg 2015; 27: 39–44.
28. Brooks JT, Yaszay B, Bartley CE, et al. Do all patients with cerebral palsy require postoperative intensive care admission after spinal fusion? Spine Deform 2019; 7(1): 112–117.
29. Murphy NA, Firth S, Jorgensen T, et al. Spinal surgery in children with idiopathic and neuromuscular scoliosis. What’s the difference? J Pediatr Orthop 2006; 26(2): 216–220.
30. Barsdorf AI, Sproule DM and Kaufmann P. Scoliosis surgery in children with neuromuscular disease: findings from the US National Inpatient Sample, 1997 to 2003. Arch Neurol 2010; 67(2): 231–235.
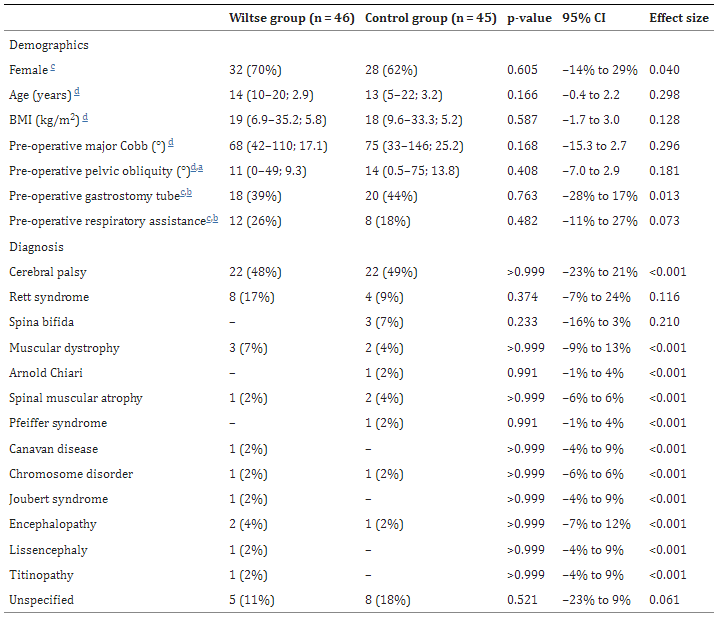
Figure 1
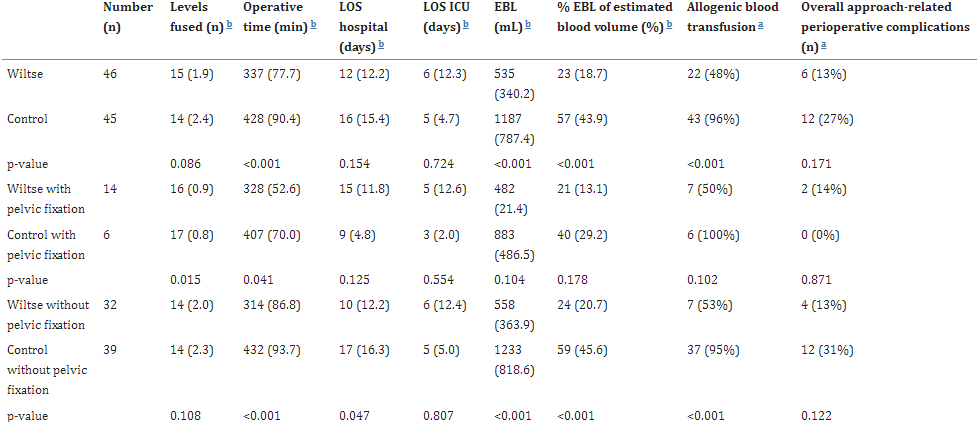
Figure 2
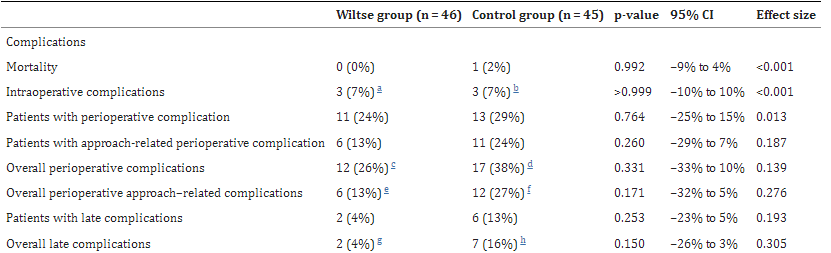
Figure 3
