Diagnostic Pitfalls in Actinomycosis: Case Report of a Deep-Seated Thigh Mass Mimicking Malignancy
Diagnostic Pitfalls in Actinomycosis: Case Report of a Deep-Seated Thigh Mass Mimicking Malignancy
Ali Ijaz Ahmad *, Ilkyu Han 1
1. MD, PHD Professor, Department of Orthopaedic Surgery, Seoul National University Hospital, 101 Daehak-ro Jongno- gu, 03080 Seoul, Korea. Department of Orthopaedic Surgery, Seoul National University College of Medicine, 101 Daehak-ro Jongno-gu, 03080 Seoul, Korea.
*Correspondence to: Ali Ijaz Ahmad, MBBS, FCPS (Orth), MRCS, Clinical Fellow Orthopedic Oncology, Department of Orthopaedic Surgery, Seoul National University Hospital, 101 Daehak-ro Jongno- gu, 03080 Seoul, Korea.
Copyright
© 2024 Ali Ijaz Ahmad. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 24 Sep 2024
Published: 01 Oct 2024
Abstract
While typically associated with cervicofacial and thoracoabdominal infections, Actinomycosis, a chronic bacterial infection, can manifest in various ways, occasionally mimicking malignancy. This case report describes a 60-year-old woman presenting with an 8-month history of a progressively enlarging left thigh mass and weight loss. Imaging studies (MRI and FDG-PET) revealed a concerning soft tissue mass with features suggestive of malignancy. Initial core needle biopsy results pointed towards a myofibroblastic tumor. However, wide surgical excision and subsequent histopathological examination with special stains identified sulphur granules with Actinomycotic colonies and filamentous structures, confirming the diagnosis of Actinomycosis involving the left thigh muscle. This case emphasizes the importance of considering Actinomycosis in the differential diagnosis of soft tissue masses and maintaining a high index of suspicion for Actinomycosis, even in atypical presentations, is crucial for optimal patient care.
Keywords: histopathological examination, mimick, malignancy, soft tissue mass, actinomycosis
Diagnostic Pitfalls in Actinomycosis: Case Report of a Deep-Seated Thigh Mass Mimicking Malignancy
Introduction
Actinomycosis, a chronic granulomatous infection caused by Actinomyces spp., is an uncommon disease with a propensity to mimic malignancy. While Actinomyces israelii is a constant resident of the human oral cavity, gastrointestinal, and genital tracts, it is unable to breach a healthy mucosal barrier. Therefore, infection typically occurs only in the context of underlying conditions that compromise this barrier. These conditions can include trauma, surgery, or the presence of a foreign body. Clinicians are now familiar with classic presentations such as cervicofacial involvement (50-65%) following dental procedures, abdominal (20%), thoracopulmonary (15-20%), and pelvic involvement in women using intrauterine devices (IUDs), as well as various rare anatomical sites such as cutaneous, CNS and soft tissues, often mimicking the clinical and imaging features of malignancy or tuberculosis, posing a significant diagnostic challenge [1, 2].
The cornerstone of diagnosis relies on a high index of suspicion by the treating physician and confirmation by both microbiology and pathology. Bacterial cultures require prolonged incubation under anaerobic conditions to optimize the growth of Actinomyces spp. Histopathological examination demonstrates characteristic findings such as necrosis with sulfur granules and filamentous, gram-positive, branching bacteria with a morphology resembling fungi [3]. These criteria are essential for establishing an accurate diagnosis of actinomycosis. We herein report on a rare presentation of actinomycosis which was treated with surgical intervention and antibiotics.
Case Report
A 60-year-old woman with no significant past medical history presented with an 8-month history of a progressively enlarging left medial thigh mass. She also reported a weight loss of 3 kg over the past 3 months. Physical examination revealed a palpable left thigh mass with no signs of skin inflammation or drainage.
Magnetic resonance imaging (MRI) revealed a 4.7x7.2x9 cm irregular soft tissue mass in the left medial proximal thigh involving the adductor magnus muscle. The mass demonstrated intermediate and heterogeneous T2 signal intensity with an irregular peripheral T2 dark signal rim and intermediate T1 signal intensity. Additionally, the MRI showed extensive surrounding muscle and subcutaneous edema with a branch of the deep femoral artery coursing through the mass. Gadolinium-enhanced images revealed multilocular cystic areas surrounded by intense heterogeneous enhancement of the solid components. The mass demonstrated features concerning for malignancy [Figure 1, 2, 3, 4]. A fluorodeoxyglucose (F-18 FDG) PET scan demonstrated mildly hypermetabolic lymph nodes in the left inguinal region (suspected reactive) and a few small inflammatory nodules without FDG uptake in both lungs, but no evidence of distant metastasis [Figure 5].
In the current study, inflammatory markers, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), were elevated (ESR: 71 mm/hr; normal range: 0-15 mm/hr; CRP: 3.49 mg/L; normal range: <3 mg/L). Core needle biopsy revealed a myofibroblastic tumor with low to intermediate grade and mild to moderate increased cellularity. The biopsy also showed mild nuclear pleomorphism, no necrosis, and 0/10 HPF mitoses.
FIGURE 1: Axial T1-weighted MR image Intermediate T1 signal intensity of the medial thigh mass involving the adductor magnus muscle
FIGURE 2: Axial T1-weighted fat-saturated gadolinium-enhanced image Multilocular cystic areas in central part of lesion surrounded by intense heterogeneous enhancement of the solid elements
FIGURE 3: Axial T2-weighted MR image Mass appearing with intermediate and heterogeneous signals
FIGURE 4: Coronal T2-weighted MR image Mass in adductor compartment of thigh with intermediate and heterogeneous signals
Wide margin excision and neurolysis of sciatic and femoral nerves was performed, resulting in a 22.0x12.0x10.5cm specimen with negative margins (frozen section) sent for histopathological evaluation. Gross examination revealed a grayish-white solid mass within the muscle layer [Figure 6, 7]. Microscopic examination demonstrated necrosis, abscess formation, and extensive reactive granulation tissue formation.
FI GURE 5: FDG-PET Hypermetabolic lesion in adductor compartment of thigh
FIGURE 6 (left): Gross Specimen Proximal (black arrow) and distal (white arrow) margins of resection
FIGURE 7 (right): Cut section Central necrosis (white arrow) with grey-white appearance of the surrounding part of mass
Notably, sulphur granules with actinomycotic colonies, filaments and club shaped structure (Speldore-Hoeppli reaction) were identified along within the abscess cavity [Figure 8, 9, 10]. The previously identified myofibroblasts on biopsy were attributed to reactive fibroblasts surrounding the abscess. Immunohistochemistry showed positivity for Ki-67 in 29.1% of cells and a few scattered IgG4-positive cells. ALK (5A4) and MUC-4 stains were negative.
FIGURE 8: Histopathology Spindle cell proliferative lesion
FIGURE 9: Sulphur granule Sulphur granule (black arrow) shown is composed of masses of gram-positive bacteria with branching filaments and eosinophilic amorphous material with club shaped configuration surrounding the granule (Splendore-Hoeppli reaction).
FIGURE 10: Sulphur granule Magnified view of sulphur granule and Splendore- Hoeppli reaction
PAS staining revealed filamentous structures consistent with Actinomyces, and Gram stain confirmed the presence of gram-positive branching bacteria. Based on the histopathological findings with identification of Actinomyces colonies and supportive special stains, the diagnosis of Actinomycosis of the left thigh muscle was established. The patient received appropriate antibiotic therapy for Actinomycosis. Long-term follow up remained uneventful with no recurrence or complication
Discussion
In understanding Actinomycosis, it's crucial to recognize its diverse manifestations and diagnostic challenges. Actinomycosis, caused by Actinomyces species, is a rare but significant condition often misdiagnosed due to its ability to mimic neoplastic processes. Through the analysis of this case report and the insights from related literature, we underscore the diagnostic challenges and therapeutic considerations associated with Actinomycosis masquerading as a soft tissue tumor of the thigh.
Actinomycetes, particularly Actinomyces Israelii, inhabit various niches in the human body, notably the oral and vaginal microbiota, where they primarily act as commensals. While Actinomycosis commonly affects the head and neck, thorax, or abdomen, it may also manifest in extremities, albeit less frequently, either independently or alongside thoracoabdominal or disseminated infections. Cervicofacial involvement (50-65%), often following dental procedures, remains well-documented, followed by abdominal (20%) and thoracopulmonary regions (15-20%). However, atypical presentations, such as pelvic involvement in women using intrauterine devices (IUDs), or involvement of the central nervous system (CNS), skin, and soft tissues, have also been increasingly recognized. The disease, although global, exhibits no clear demographic patterns, with peak incidence observed in middle decades of life [4].
Cutaneous actinomycosis, for instance, can mimic nodular lesions or subcutaneous abscesses resembling skin tumors, adding to the diagnostic complexity [5, 6]. Similarly, CNS involvement can present with symptoms akin to brain tumors or meningitis, while soft tissue infections may mimic abscesses or malignancies (7). The deceptive nature of Actinomycosis, marked by its indolent course, nonspecific clinical features and ability to spread across tissue planes, forming masses, often leads to misdiagnosis as cancer [8].
This case parallels previous reports where Actinomycosis presented in atypical deep seated locations in soft tissues, such as the thigh and para-iliac regions, challenging the conventional perception of its primary sites of manifestation [2, 9-12] (Table 1).
Literature highlights the diverse clinical spectrum of Actinomycosis, often manifesting as chronic abscesses with nonspecific systemic symptoms. Notably, Actinomycosis without a clear entry point for the organism such as trauma or bites has been documented in literature, emphasizing the insidious nature of the infection and its ability to develop in seemingly unaffected tissues [13]. This heterogeneity complicates diagnosis, as symptoms may overlap with those of neoplastic processes, tuberculosis, or inflammatory conditions.
MRI findings of actinomycosis in various anatomical locations remain largely variable and nonspecific.
However, MRI may aid in delineating the extent of involvement and guiding biopsy for histopathological confirmation.16 In extremity involvement, such as the thigh as discussed in this case report, it commonly presents as heterogeneous infiltrative well defined masses with low signal intensity on T1-weighted MR images, high intensity signal on T2-weighted MR images and moderate contrast enhancement, with non-enhancing portions suggesting central necrosis, often mimicking neoplastic processes. Similar finding have been seen in craniofacial/ mandibular actinomycosis [10-12, 14, 15].
Interestingly, however, some thoracic/ mediastinal and abdominal actinomycosis have been reported with prominent fibrotic tissue, the inflammatory stranding and the solid component of the mass tend to demonstrate intermediate to low signal intensity on T2-weighted MR images. Additionally, contrast-enhanced T1-weighted MR images show avid enhancement of the surrounding inflammatory infiltrations, as well as a solid portion in the mass.
|
Case no. |
Author, Year [reference] |
Age/se x |
Site |
Bone involvemen t |
Skin involvemen t |
Muscle involvemen t |
Cultur e |
Biops y |
LN involvemen t |
Treatment |
|
1 |
Reiner et al., 1987 [2] |
30/M |
thigh |
+ |
+ |
+ |
+ |
+ |
+ |
Surgery and Antibiotics |
|
2 |
Navarre et al., 2014 [9] |
15/F |
para- iliac |
- |
- |
+ |
+ |
+ |
- |
Surgery and Antibiotics |
|
3 |
Vishwanathan et al., 2013 [10] |
69/M |
thigh |
- |
- |
+ |
NA |
+ |
- |
Antibiotics only |
|
4 |
Kumar et al., 1991 [11] |
14/M |
above knee |
- |
- |
+ |
+ |
+ |
- |
Surgery and Antibiotics |
|
5 |
Khandelwal et al., 2012 [12] |
42/F |
thigh |
- |
+ |
+ |
- |
+ |
- |
Surgery and Antibiotics |
TABLE 1: Comparison of Deep-Seated Actinomycosis Cases Mimicking Malignancy in Prior Case Reports
"+" = Positive, "-" = Negative, "NA" = Not Available
Registered diffusion, perfusion MR and MR spectroscopy have been studied in brain and pelvic actinomycosis.
MR spectroscopic features (suggestive of abscesses including elevated peaks of amino acids, lactate, alanine, acetate, pyruvate and succinate and absent signals of N-acetyl aspartate, creatine and choline), restricted diffusion and low apparent diffusion coefficient (ADC) have been of value primarily to distinguish actinomycotic abscesses from cystic brain tumors, but are not specific for actinomycosis [17].
However, given the potential overlap with other infectious or neoplastic conditions, histopathological examination remains imperative for definitive diagnosis despite the utility of MRI, revealing characteristic colonies (sulphur granules) formed by tangled filaments surrounded by radiating, sometimes clubbed, organisms. These filamentous, gram-positive, anaerobic-to-microaerophilic bacteria and PAS-positivity. Metagenomic next-generation sequencing (mNGS) is also a promising new molecular biological detection technology that can be employed in doubtful cases [18]. Serological tests for Actinomycosis are still under development and hold promise for non-invasive diagnosis, but their sensitivity and specificity remain to be optimized compared to traditional methods [19].
Therapeutic management of Actinomycosis typically involves prolonged antibiotic therapy, with penicillin being the mainstay. Tailoring the dosage and treatment duration (usually 6-12 months) to the severity, location, and individual patient factors is crucial for optimal outcomes. For patients allergic to penicillin, alternative antibiotics like sulfonamides, doxycycline, tetracycline or erythromycin can be considered, though with careful monitoring due to potential side effects [20]. With prompt diagnosis and appropriate therapy, Actinomycosis generally carries a favorable prognosis. Long-term follow-up is essential to ensure complete eradication and prevent recurrences, which can occur in up to 20% of cases if not adequately treated. Surgical intervention may be warranted in extensive or refractory cases, emphasizing the importance of a multidisciplinary approach to optimize patient outcomes.
Conclusion
This case report and review of the literature illuminate the diagnostic complexities of Actinomycosis. Clinicians must maintain a high index of suspicion for this elusive infection, especially in soft tissue masses exhibiting chronic progression and tissue invasion. Comprehensive diagnostic tools are essential, but definitive diagnosis relies on histopathological examination. Tailored antibiotic therapy remains the cornerstone of treatment, with surgery reserved for specific cases. Our unique presentation of Actinomycosis mimicking a skeletal muscle tumor highlights the need for further documentation of such cases to refine diagnostic criteria and inform future treatment strategies. Ultimately, prompt recognition and accurate diagnosis are paramount for optimizing patient management and outcomes.
Additional Information
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
1. Boyanova L, Kolarov R, Mateva L, Markovska R, Mitov I. Actinomycosis: a frequently forgotten disease. Future Microbiol. 2015 Apr;10(4):613-28.
2. Reiner SL, Harrelson JM, Miller SE, Hill GB, Gallis HA. Primary actinomycosis of an extremity: a case report and review. Rev Infect Dis. 1987 May-Jun;9(3):581-98.
3. Bennhoff DF. Actinomycosis: diagnostic and therapeutic considerations and a review of 32 cases.
Laryngoscope. 1984 Sep;94(9):1198-217.
4. Belmont MJ, Behar PM, Wax MK. Atypical presentations of actinomycosis. Head Neck. 1999 May;21(3):264- 8.
5. Gupta V, Jain P, Gupta G, Gupta S, Gill M, Singh S. Primary cutaneous actinomycosis of upper extremity masquerading as soft tissue neoplasm: a case report. Trop Doct. 2012 Jan;42(1):58-9.
6. Ngow H, Khairina WW. Cutaneous actinomycosis: the great mimicker. J Clin Pathol. 2009 Aug;62(8):766.
7. Ravindra N, Sadashiva N, Mahadevan A, Bhat DI, Saini J. Central nervous system actinomycosis—a clinicoradiologic and histopathologic analysis. World Neurosurg. 2018 Jan;116.
8. Acevedo Claros FN, Baudrand Biggs R, Letelier Saavedra LM, Gaete P. Actinomycosis: a great pretender.
Case reports of unusual presentations and a review of the literature. 2008.
9. Navarre P, Cantin MA, Isler MH. Para-iliac actinomycetoma presenting as sarcoma, a late complication of appendicitis: a case report. Int J Surg Case Rep. 2014;5(2):43-6.
10. Vishwanathan B, Ganesh M, Kavitha R, Pinnelli VBK. Actinomycosis masquerading as soft tissue tumor of the thigh: a rare case report. Int J Clin Diag Res. 2013;1(1):1-6.
11. Kumar A, Detrisac DA, Krecke CF, Jimenez MC. Actinomycosis of the thigh presenting as a soft-tissue neoplasm. J Infect. 1991 Sep;23(2):187-90.
12. Khandelwal R, Jain I, Punia S, Singh A, Yadav S, Sharma P, et al. Primary actinomycosis of the thigh–a rare soft tissue infection with review of literature. JRSM Short Rep. 2012 Apr;3(4):21.
13. Valour F, Sénéchal A, Dupieux C, Karsenty J, Lustig S, Breton P, et al. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183-97.
14. Demirhan S, Orner E, Szymczak W, Lee PJ, Aldrich M. Skin and Soft Tissue Actinomycosis in Children and Adolescents. Pediatr Infect Dis J. 2024;43(1):10.1097.
15. Fisch C, Schmutz G, Benko A, Kastler B. Mediastinal and heart wall invasion by actinomycosis: CT and MRI appearances. Eur Radiol. 1994;4(2):175-8.
16. Heo SH, Shin SS, Kim JW, Lim HS, Seon HJ, Jung SI, et al. Imaging of actinomycosis in various organs: a comprehensive review. Radiographics. 2014 Jan-Feb;34(1):19-33.
17. Wang S, Wolf RL, Woo JH, Wang J, O’Rourke DM, Roy S, et al. Actinomycotic brain infection: registered diffusion, perfusion MR imaging and MR spectroscopy. Neuroradiology. 2006 Apr;48(5):346-50.
18. Wang W, Ren D, Xu C, Yuan Q, Zhang Q, Hu H, et al. Pulmonary actinomycosis diagnosed by radial endobronchial ultrasound coupled with metagenomic next-generation sequencing: a case report and brief literature review. Int J Infect Dis. 2020 Aug;100:379-81.
19. Cantres-Fonseca OJ, Vando-Rivera V, Fonseca-Ferrer V, Latorre CC, Del Olmo-Arroyo FJ. Actinomycosis: diagnosis, clinical features and treatment. In: Actinobacteria-Diversity, Applications and Medical Aspects. IntechOpen; 2022.
20. de Leoz JB, Suravajjala D, Rafeek H, Selvan V. Primary mammary actinomycosis challenged with penicillin allergy. BMJ Case Rep CP. 2021 Jul;14(7).
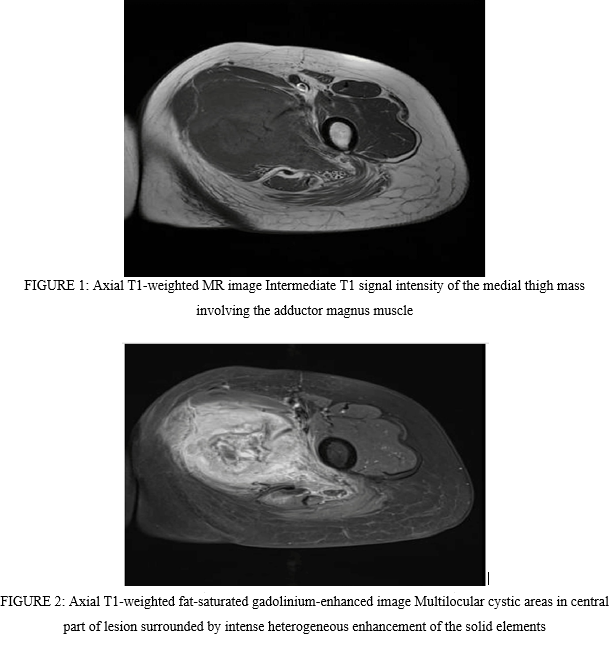
Figure 1
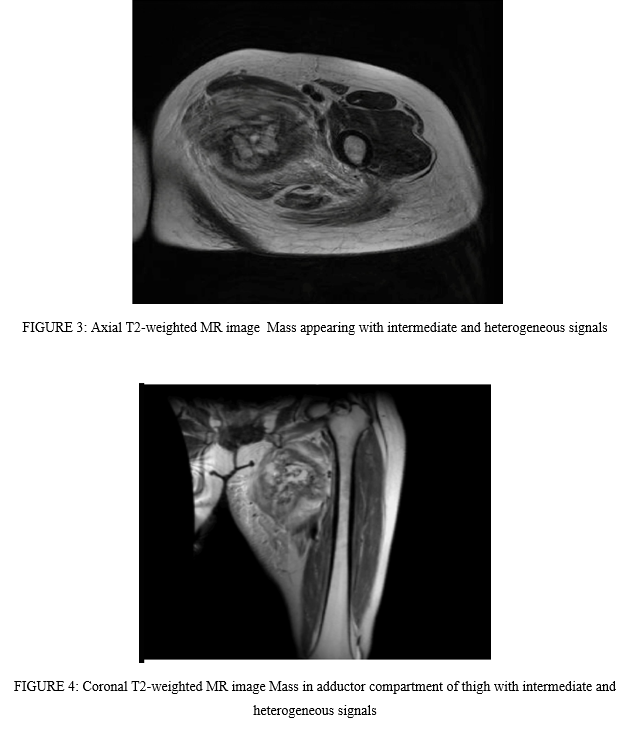
Figure 2
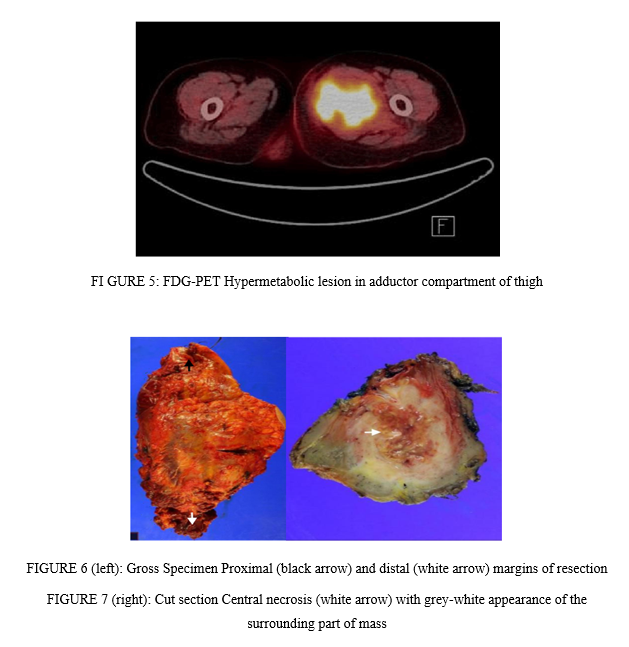
Figure 3
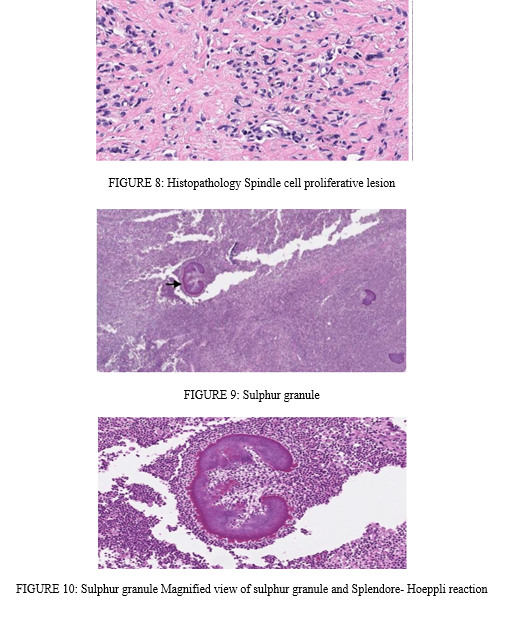
Figure 4
