A Systematic Review and Meta-Analysis of Total Knee Replacements Using Robotics Versus Conventional Techniques
A Systematic Review and Meta-Analysis of Total Knee Replacements Using Robotics Versus Conventional Techniques
Syed Muhammad Tayyab Hassan *
*Correspondence to: Syed Muhammad Tayyab Hassan. Registrar Orthopedic Surgery, Allied Hospital & Punjab Medical College Faisalabad, Pakistan.
Copyright
© 2021 Syed Muhammad Tayyab Hassan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 15 January 2021
Published: 27 January 2021
Abstract
Robotic knee replacement surgery has become a new trend that has attracted the attention of orthopedic surgeons worldwide. For example, the use of robots can increase the accuracy of positioning and customization. The aim of this study is to compare the evidence between robotic total knee arthroplasty and conventional techniques, focusing on radiographic images and study results. A randomized controlled trial (RCT) was conducted on January 1, 2022, specifically to compare the outcomes of robotic and conventional total knee arthroplasty. We were interested in outcomes such as knee range of motion, Medical and Functional Knee Society scores, Western Ontario and McMaster Universities scores (WOMAC), Hospital for Scores Medical Specialties, complications, and radiographic difficulties. This review was conducted in accordance with the International Systematic Review and Meta-Analysis guidelines. We assessed the risk of bias using the revised Cochrane risk of bias for randomized trials (RoB 2). Of these knees, 974 received a robotic arm and the remaining 968 received a knee-based implant. Our results showed that the robotic knee was used in postoperative treatment (OR ≤ 0.82; 95% CI, ≤ 1.027 to ≤ 0.58, p-value <0.00001) and mechanical treatment (OR ≤ 0.95; 95% CI, ≤ 1.49 to ≤ 0.41, p-value <0.0006). knee joint motion (OR≤2.23; 95% CI≤4.89≤0.43, p-value 0.1) and femoral component position (OR≤0.98; 95% CI, ≤2.03 Ø0.08, p-value 0.07). Clinical, functional outcomes and complications were similar between the robotic surgery and knee surgery groups. It provides superior postoperative anatomical and mechanical adaptation compared to conventional surgery. However, clinical and functional outcomes and associated complications were similar. These findings should be evaluated in the context of potential confounding. More controlled studies using new robotic systems are needed to confirm the optimal performance and clinical outcomes of robotic surgery.
Keywords: Total knee arthroplasty · Robotic arthroplasty · Jig-based arthroplasty · Conventional knee arthroplasty
A Systematic Review and Meta-Analysis of Total Knee Replacements Using Robotics Versus Conventional Techniques
Introduction
Total knee replacement has experienced significant growth in recent decades, with the UK recording 312,167 primary knee replacements from 2017 to 2019. This surge is largely due to the increasing prevalence and economic impact of osteoarthritis among different populations. Despite the effectiveness and replicability of traditional knee arthroplasty methods and advancements in prosthesis technology, many patients are still unhappy with their knee replacements due to factors such as soft tissue balance and implant placement.
Conventional total knee arthroplasty (CTKA) is often effective but can be challenging and intricate to obtain, especially in more complex cases. The development of robotic total knee arthroplasty (RTKA) aims to eliminate potential inaccuracies in implant positioning and alignment, reducing patient dissatisfaction. The first RTKA was performed in the UK in 1988 using the Acrobat system. Most robotic systems used in knee arthroplasty use 3D imaging, suggesting they offer higher precision in positioning and balancing. Some reports even suggest they outperform traditional jig-based methods in clinical settings.
Various robotic arms have been developed and incorporated into medical practice over the past decades, including ROBODOC, Mako, CASPAR, and NAVIO. This meta-analysis aims to provide the most robust evidence currently available to compare robotic total knee arthroplasty with its conventional equivalent in the existing literature.
Materials and Methods
This meta-analysis was conducted using the PRISMA checklist and algorithm, focusing on original comparative level I of evidence randomized controlled trials (RCTs) reporting primary total knee arthroplasty (TKA) in robotic total knee arthroplasty with its conventional equivalent. The study included studies involving patients with infammatory arthritis or post-traumatic arthritis, non-comparative or not reporting outcomes, review articles, cross-sectional, case series, and reports, and preclinical or animal studies. Data was collected using a pre-designed data collection sheet in Microsoft Excel, including surname of the first author, year of study, age, gender, patient count, prosthesis type, robotic system used, points of follow-up, revision rates for any cause, and complications encountered.
The study evaluated several outcomes of interest, including scores for knee society pain and function, the Western Ontario and McMaster University score (WOMAC), the Hospital of Special Surgery score (HSS), knee range of motion, and alignment parameters. Data related to sagittal and coronal knee alignments were also obtained. The qualitative analysis was conducted using the revised Cochrane risk-of-bias tool for randomized trials (RoB 2), which evaluates five key areas: randomization, adherence to intended treatments, missing outcomes, measurement bias, and reporting bias.
The meta-analysis was performed using RevMan V.5.0.18.33, extracting mean and standard variations to present continuous variables, analyzing dichotomous variables by relative risk (RR) with 95% CI, measuring heterogeneity using I2, and considering results statistically significant at p<0.05.
Results
The study selection process involved a search of 651 articles, with 318 being duplicates and 79 being excluded. The remaining articles were screened based on title and abstract, resulting in the exclusion of 79. The full text of the 333 remaining articles was evaluated against the inclusion criteria, resulting in seven studies meeting the eligibility criteria.
The study included 1942 knees, with 974 being implanted using robotic arms and the remaining 968 being conventionally implanted. All TKAs in the included RCTs were cemented. In terms of robotic systems, five papers [18–22] utilized the ROBODOC system (Integrated Surgical Systems, Sacramento, CA) for the robotically assisted knee group, while the other two studies [23, 24] used the NAVIO® system (Smith and Nephew, Andover, TX, USA). All trials included in the study matched their study groups in terms of participant age and gender. However, there was a variation in the follow-up periods, so the researchers reported their results at the final follow-up.
Table 1: Characteristics of the studies
Three studies demonstrated a low risk of bias, while five studies exhibited some concern for bias. Notably, none of the included studies showed a high risk of bias. All studies maintained their groups according to the original randomization, and no study experienced a high dropout rate or failed to report outcomes.
|
Study Mean SD total Mean SD Total Weight Mean Difference |
|
2016 81.8 14.9 31 87.9 10.6 28 8.7% 6.10 (-12.65, 0.45) 2007 91.6 2.94 32 90.9 4.88 30 91.3% 0.70 (-1.82, 2.72) |
Table 2: clinical knee society score at the fnal follow up between RTKA and CTKA,
CI confidence interval.
The clinical knee society score (KSS clinical) was documented in two studies [19, 20], which reported their outcomes at varying follow-up periods, ranging from 24 to 47 months. The meta-analysis outcome at the final follow-up showed no statistically significant difference between the two groups. The functional knee society score (KSS functional) was outlined in two studies [19, 20], which demonstrates no statistical difference between the two groups.
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) functional score was examined in two papers [21, 22], with neither reporting any differences between RTKA and CTKA at 12 and 36 months, respectively.
Four studies [19–22] reported on the post-operative range of motion, with their analysis being conducted at the final follow-up, which ranged from 12 to 47 months. The fxed effect meta-analysis indicated a superiority of RTKA knees in terms of range of motion; however, this was not statistically significant.
Post-operative alignment parameters were extensively studied in the included papers. The tibiofemoral and mechanical axes were reported in three studies each. The robotic knee was statistically superior in restoring the tibiofemoral and mechanical axes, respectively. However, the results for the tibiofemoral axis demonstrated high heterogeneity. On the other hand, other parameters such as the female fexion angle, anteroposterior and lateral tibial angles were reported in six studies [18, 20–24]. Our fxed model analysis did not reveal any signifcant differences between the anteroposterior and lateral tibial angles in both knee arthroplasty techniques (p value > 0.05).
Discussion
The rise in knee replacement surgeries, primarily due to osteoarthritis, has advanced both conventional and robotic techniques. However, achieving optimal patient satisfaction remains a challenge, with precise implant placement and soft tissue balance being key factors. Robotic Total Knee Arthroplasty (RTKA) emerged to address these issues, promising enhanced accuracy. A meta-analysis was crucial as it sought to compare RTKA with CTKA methods. The most significant result from this meta-analysis was the markedly improved restoration of mechanical alignment in robotic-assisted knee arthroplasty compared to jig-based methods. This finding, which was a unique outcome of our level I study, could likely be credited to the accuracy of knee balancing in robotic surgeries. Furthermore, our study findings concur with prior acknowledgments concerning the superior performance of robotic-assisted knee arthroplasty in terms of implant placement and reduction of radiological outliers.
The precision of robotic knees concerning balancing and implant placement has been shown to positively influence knee outcomes in a few cohorts. However, this meta-analysis was unable to demonstrate any superiority in patient-reported outcome scores. The introduction of kinematic alignment, which can be replicated in robotic knees, has increased the popularity of robotic arthroplasty among surgeons. While kinematic alignment seems to be a promising direction for knee balancing, no long-term studies currently confrm its superiority over other balancing techniques. On the other hand, while RTKA promises theoretical precision, the substantial learning curve and extended operative times present notable concerns. The requirement for preoperative CT imaging with certain systems further adds to the duration, cost, and radiation exposure, complicating its widespread adoption.
While robotics may yield improved clinical and radiological outcomes, it is necessary to weigh these potential benefits against the increased cost of robotic surgery. Certain robotic systems employ CT scans, which can further escalate costs. Several studies have estimated an increased cost per knee of $1000-1350, and this does not take into account any additional radiological studies that may be required.
Conclusion
The meta-analysis suggests that robotic total knee replacements offer better post-operative anatomical and mechanical alignment than conventional total knee replacements. However, clinical and functional outcomes and complication rates are similar. The study suggests further randomized controlled trials with the latest robotic systems to confirm superior functional and clinical outcomes.
Reference
1. Ben-Shlomo Y, Blom A, Boulton C (2020) The national joint registry 17th annual report 2020 [Internet]. National Joint Registry, London
2. Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL, Laslett LL, Jones G, Cicuttini F, Osborne R, Vos T, Buchbinder R, Woolf A, March L (2014) The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 73(7):1323–1330
3. Choi YJ, Ra HJ (2016) Patient satisfaction after total. Knee Arthroplasty Knee Surg Relat Res 28(1):1–15
4. Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE (2018) Patient satisfaction after total knee replacement: a systematic review. HSS J 14(2):192–201
5. Clement ND, Calliess T, Christen B, Deehan DJ (2020) An alternative technique of restricted kinematic alignment of the femur and gap balanced alignment of the tibia using computer aided navigation. Bone Jt Res 9(6):282–284
6. Meloni MC, Hoedemaeker RW, Violante B, Mazzola C (2014) Soft tissue balancing in total knee arthroplasty. Joints 2(1):37–40
7. Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus–valgus balance and range of movement after total knee arthroplasty. J Bone Jt Surg Br 87(6):804–808
8. Jakopec M, Harris SJ, Rodriguez y Baena F, Gomes P, Cobb J, Davies BL (2001) The frst clinical application of a “hands-on” robotic knee surgery system. Comput Aided Surg 6(6):329–339
9. Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR (2013) Predicting the cost-efectiveness of total hip and knee replacement: a health economic analysis. Bone Jt J 95(1):115–121
10. Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA (2018) Robotic arm-assisted total knee arthroplasty. J Arthroplasty 33(7):2002–2006
11. Agarwal N, To K, McDonnell S, Khan W (2020) Clinical and radiological outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 35(11):3393-3409.e2
12. Think surgical (2022) https://thinksurgical.com. Accessed 20 Oct 2022
13. “Mako.” Stryker (2022) https://www.stryker.com/us/en/portfolios/Orthopedics/joint-replacement/mako-robotic-arm-assisted-surgery.html. Accessed 20 Oct 2022
14. Minimally invasive surgery in orthopedics (2012) Springer, New York
15. NAVIO Surgical System - Robotics-assisted Knee Replacement | Smith & Nephew (2022) https://www.smith-nephew.com/professional/microsites/navio/. Accessed 20 Oct 2022
16. Liberati A, Altman DG, Tetzlaf J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-Analyzes of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
17. Sterne JAC, Savovi? J, Page MJ, Elbers RG, Blencowe NS, Boutron I (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
18. Kim YH, Yoon SH, Park JW (2020) Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized controlled trial. Clin Orthop Relat Res 478(2):266–275
19. Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ (2017) Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 25(9):2942–2951
20. Park SE, Lee CT (2007) Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 22(7):1054–1059
21. Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW (2011) Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 19(7):1069–1076
22. Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 471(1):118–126
23. Thiengwittayaporn S, Uthaitas P, Senwiruch C, Hongku N, Tunyasuwanakul R (2021) Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: a randomized controlled trial. Int Orthop 45(11):2851–2858
24. Vaidya NV, Deshpande AN, Panjwani T, Patil R, Jaysingani T, Patil P (2022) Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 30(2):621–626
25. Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL (2014) Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty 29(12):2373–2377
26. Jefery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Jt Surg Br 73(5):709–714
27. Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS (2003) Factors afecting the durability of primary total knee prostheses. J Bone Jt Surg Am 85(2):259–265
28. Decking J, Theis C, Achenbach T, Roth E, Nafe B, Eckardt A (2004) Robotic total knee arthroplasty: the accuracy of CTbased component placement. Acta Orthop Scand 75(5):573–579
29. Hantouly AT, Ahmed AF, Alzobi O, Toubasi A, Salameh M, Elmhiregh A, Hameed S, Ahmed GO, Alvand A, Al Dosari MAA (2022) Mobile-bearing versus fxed-bearing total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 32(3):481–495
30. Elmhiregh A, Abuodeh Y, Alzobi O, Zikria B, Alkhayarin M, Morrey BF (2023) All-polyethylene versus metal-backed tibial components in total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 33:3611–3622.
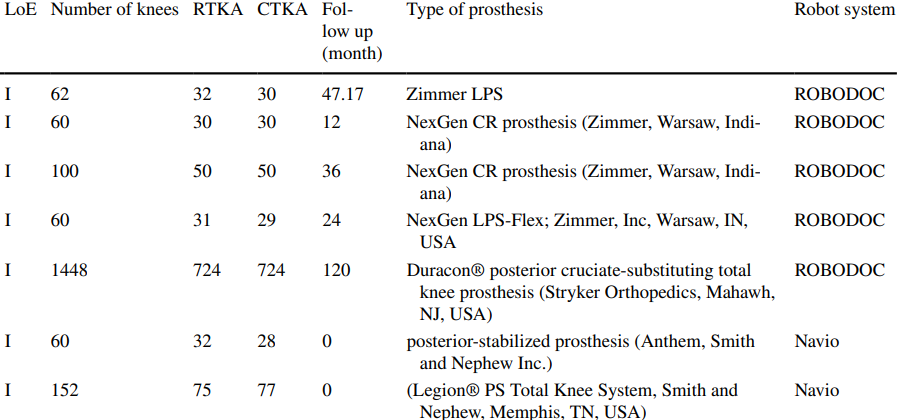
Figure 1
