An Analysis of 100 Cases of Ultrasound-Guided medical Branch Block of lumbar facet in a Referral Centre.
An Analysis of 100 Cases of Ultrasound-Guided medical Branch Block of lumbar facet in a Referral Centre.
Dr.R.Barani *
*Correspondence to: Dr.R.Barani MS, DNB(ortho), MNAMS,MRCS(Ed), Fellow spine (France/ S.Korea), Consultant spine surgeon, Apollo hospitals, Chennai, India.
Copyright
© 2024 Dr.R.Barani. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 20 Aug 2024
Published: 18 Oct 2024
Abstract
This study aims to demonstrate the effectiveness of ultrasound-guided blockade of the medial branches of dorsal rami of lumbar facet joints in patients with facetal arthritis syndrome. Age, gender, laterality, and pain relief using visual analogue scale (VAS) were calculated. All patients had ultrasound-guided block injection with drugs: 2% lidocaine (without vasoconstrictor) + methylprednisolone acetate (40mg). The mean age of the patients was 61 years, the youngest was 32 and the oldest was 93 years. Predominantly women were affected due to facet pain ( 60% female : 40 % male ). 13% of the patients had single level , 67% had two levels affected, and 20% had three levels affected. There was a significant improvement in VAS scale for axial pain following USG guided facetal injections. Conclusion : ultrasound is effective in diagnosing facetal arthritis and providing therapeutic blocks of the medial branch of dorsal rami and facets for facet arthritis syndrome.
Keywords: ultrasound guided blocks, facetal arthritis , Low back pain.
An Analysis of 100 Cases of Ultrasound-Guided medical Branch Block of lumbar facet in a Referral Centre.
Introduction
Back pain is considered the number one reason for consulting an orthopedic surgeon worldwide. According to reports, lumbar facet joints account for 15% to 45% of patients with back pain. The medial branches of the dorsal rami of the spinal nerves innervate the facet joints and the deep erector spinae muscles. Traditionally fluoroscopy and CT scans are considered better tools to identify and treat osseous structures. Hence they were utilized often in localizing the levels and lesion in spinal pain to plan interventions including block injections to relieve pain. Of late ultrasound is gaining more importance in not only defining osseous structure but also in planning interventions with reduced radiation14,15. The ease of adaptation of the technique, accuracy, ability to perform in simple day care centers is a inherent advantage of ultrasound14-17. This research work aims at localizing the level of symptoms in facet arthritis related pain using ultrasound and giving therapeutic block to medial bundle branch in a day care Centre .
Methodology
100 patients who presented with persistent axial back pain for more than 3 months not responding to analgesics and physical therapy were included in the study. Basic demographic details like age , sex along with location of pain and severity of pain using VAS (visual analogue scale) were documented. Radiographs and MRI scans of all patients were assessed and confirmed to have facetal arthritis at single or multiple spinal segments.
A Samsung type ultrasound device, model HS 50, with a linear and convex multifrequency probe was used for this procedure.2ml of 2% lidocaine (without vasoconstrictor) with 40mg Depot medrol ( Methylprednisolone acetate ) using a 22G spinal needle was used for infiltration in the areas identified by ultrasound.
Pain assessment with VAS scale after infiltration and at 3 weeks follow up was documented in the Epi Info™ CDC application. statistical data was obtained using the Microsoft Excel and analysed using SPSS version 29.
Patient consent was taken for the intervention and documentation of pain assessment for research purposes. Institute review board’s permission was taken for the evaluation of the procedure outcome and publication.
Result
This study analysed the result of 100 cases of ultrasound guided medial branch block of dorsal rami in lumbar facet joints at the day care procedure room in apollo hospitals, chennai ,INDIA . Lumbo sacral region was scanned to identify the level of facets joints and the arthritis pattern was documented. 2ml of 2% lidocaine (without vasoconstrictor) with 40mg depot medrol ( Methylprednisolone acetate ) was infiltrated at each joint level of suspected pain and arthritis confirmed in ultrasound. 40% of the patients were male and 60% were female. The left side was involved in 14% of the patients (14 patients), and the right side in 14%. Bilateral involvement was the most common affection involving 72% of individuals.
L4/5 facets were most frequently affected. Pain scale changed from a mean value of VAS 7/10 to 2/10 after procedure at the time of discharge which was statistically significant ( t- test , p value <0.05). None of the patients had complications following the procedure like worsening of pain , allergic reaction , hypotension or delayed infection. All the patients were called for 3 weeks follow up and evaluated for pain and activity restriction. All the patients had the same pain relief comparable to immediate post procedure assessment ( VAS scale ).
FIG 1: DISTRIBUTION OF PATIENTS
FIG 2 : GENDER DISTRIBUTION
FIGURE 3 : LEVELS AFFECTED DIAGNOSED BY ULTRASOUND
FIGURE 4: CHANGE IN PAIN – VAS SCALE (1-10), PRE / 3 WEEKS POST PROCEDURE
Figure 5
Ultrasound Images of the paraspinal region with a red asterisk locating the targets in the inter apophyseal and facet valleys, where the needle is inserted in a proximal to distal fashion with a dotted arrow indicating the path.
Figure 6
Transverse ultrasound image at the L4-L5 level showing facet arthrosis comparing with magnetic resonance image in the axial T2 plane.
Discussion
The term facet joint syndrome was first described in 1933 by Ghormley RK as pain occurring in lower back ( 2 - 5 cm from midline ) that worsens on spinal extension. Facet arthritis often co-exists with degenerative disc disease which is more symptomatic and treatment is channelized towards pain generators around the disc.
Isolated facet arthritis is a rare entity. Often clinically facet pain is treated in adjunct to discogenic pain. Facet arthritis pain responds to simple measures like physical therapy, NSAIDS and rest. Only persistent pain needs intervention in the form of fluoroscopy / CT guided medial branch of dorsal rami block. Resistant forms of pain may need radiofrequency ablation which is done with fluoroscopy guidance.
Many studies have been published exploring the diagnostic and therapeutic option ever since Greher et al8 reported the target points for ultrasound-guided dual facet blockade in 2004.Ultrasound-guided medial branch and facet dual blockade can be successful at 89.5% and can be recommended as a outpatient procedure16,17. A prospective randomized clinical trial done in 2007 involving 40 patients compared lumbar ultrasound-guided facet joint injection with computed tomography and concluded that that there was no significant difference in pain and functional improvement between them 4.
Wu Tao et al18 reviewed 202 adult patients with facet joint pain evaluating and comparing the efficacy of CT/fluoroscopy-guided facet injections with ultrasound guided injections. They noted that ultrasound is capable of defining the lumbar facetal anatomy like CT scan which makes it a outpatient procedure.
In our study we noted that the anatomy of facet joints and the degenerative changes were easy identified in all the 100 patients . Based on clinical evaluation of focal tenderness and MRI findings ( effusion and joint space irregularity ) joints were isolated and injected with local anaesthetic and steroid mixture. Immediate pain relief and persistence of pain relief till the end of 3rd week confirms the accuracy and efficacy of the injection procedure.
Conclusion
Ultrasound-guided facet blocks are easily adaptable day care procedures which give comparable results to fluoroscopy guided / CT guided blocks. Efficacy, accuracy, reduced cost, reduced radiation exposure and ability to do it in out-patient services makes it a good choice for multi -level degenerative facetal arthritis syndrome related axial back pain.
Reference
1. Galiano K, Obwegeser AA, Bodner G, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med 2005; 24:33-38.
2. Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound guidance for facet joint injections in the lumbar spine: a computed tomography-controlled feasibility study. Anesth Analg. 2005;101(2):. doi:10.1213/01.ANE.0000158609.64417.93
3. Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg AnesthPain Med 2005; 30: 391-396.
4. Galiano K, Obwegeser AA, Bale R, et al. Ultrasound-guided and CT-navigation-assisted periradicular and facet joint injections in the lumbar and cervical spine: a new teaching tool to recognize the sonoanatomic pattern. Reg Anesth Pain Med 2007; 32: 254-257.
5. Galiano, Klaus MD; Obwegeser, Alois Albert MD, MS; Bodner, Gerd MD; Freund, Martin MD; Maurer, Herbert MD; Kamelger, Florian Stefan MD; Schatzer, Reinhold MS; Ploner, Franz MD Guidance by ultrasound for injections into facet joints in the lumbar spine: a feasibility study controlled by computed tomography, Anesthesia and Analgesia: August 2005 - Volume 101 - Edition 2 - p 579-583 doi: 10.1213 / 01.ANE . 0000158609.64417.93
6. Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med 2007; 32: 317-322.
7. Ghormley RK. Low back pain with special reference to facet joints with presentation of an operative procedure. JAMA. 1933; 101: 1773–1777.
8. Greher M, Scharbert G, Kamolz LP, et al. Ultrasound-guided lumbar facet nerve block: a sonoanatomic study of a new methodologic approach. Anesthesiology. 2004;100(5):1242-1248. doi:10.1097/00000542-200405000-00028
9. Greher M., Kirchmair L., Enna B., et al. Ultrasound-guided lumbar facet nerve block: accuracy of a new technique confirmed by computed tomography. Anesthesiology. 2004; 101: 1195–1200.
10. Ha DH, Shim DM, Kim TK, Kim YM, Choi SS. Comparison of ultrasound-guided and fluoroscopy-guided facet joint block in the lumbar spine. Asian Spine J. 2010; 4:15–22.
11. Helbig T, Lee CK. Lumbar facet syndrome. Spine (Phila Pa 1976) 1988; 13:61–64.
12. Jung H, Jeon S, Ahn S, Kim M, Choi Y. The validation of fluoroscopy-confirmed ultrasound-guided lumbar facet nerve blocks. Asian Spine J. Set. 2012; 6(3): 163-7. doi: 10.4184 / asj.2012.6.3.163. Epub Aug 21, 2012 PMID: 22977695; PMCID: PMC3429606.
13. Kim D, Choi D, Kim C, Kim J, Choi Y. Transverse process and branch block needles medial to the facet joint as landmarks for ultrasound-guided selective nerve root block. Clin Orthop Surg. 2013, March; 5(1): 44-8. doi: 10.4055 / cios.2013.5.1.44. Epub Feb 20, 2013 PMID: 23467334; PMCID: PMC3582870.
14. La Grange P, Foster PA, Pretorius LK. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block. Br J Anaesth. 1978;50(9):965-967. doi:10.1093/bja/50.9.965
15. Loizides A, Peer S, Plaikner M, et al. Ultrasound-guided injections in the lumbar spine [published correction appears in Med Ultrason. 2011 Jun;13(2):178]. Med Ultrason. 2011;13(1):54-58.
16. Shi W, Tian D, Liu D, Yin J, Huang Y. The comparison of measurement between ultrasound and computed tomography for abnormal degenerative facet joints: A STROBE-compliant article. Medicine (Baltimore). 2017;96(31):e7680. doi:10.1097/MD.0000000000007680.
17. Ye L, Wen C, Liu H. Ultrasound-guided versus low dose computed tomography scanning guidance for lumbar facet joint injections: same accuracy and efficiency. BMC Anesthesiol. 2018;18(1):160. Published 2018 Nov 7. doi:10.1186/s12871-018-0620-7
18. Wu T, Zhao WH, Dong Y, Song HX, Li JH. Effectiveness of Ultrasound-Guided Versus Fluoroscopy or Computed Tomography Scanning Guidance in Lumbar Facet Joint Injections in Adults With Facet Joint Syndrome: A Meta-Analysis of Controlled Trials. Arch Phys Med Rehabil. 2016;97(9):1558-1563. doi:10.1016/j.apmr.2015.11.013.
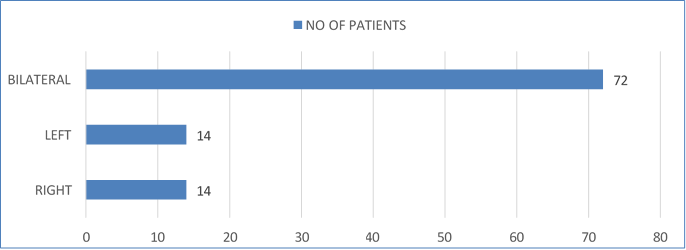
Figure 1
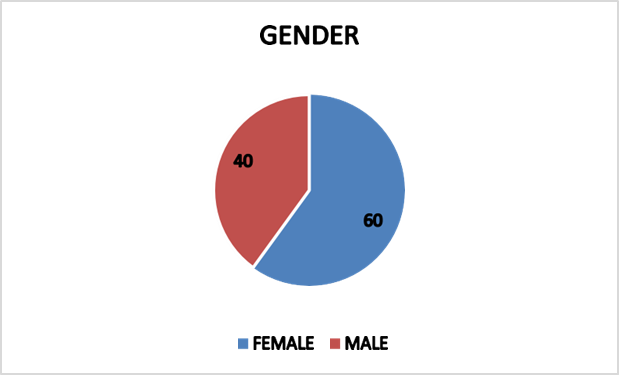
Figure 2
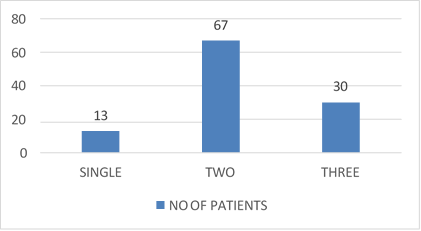
Figure 3
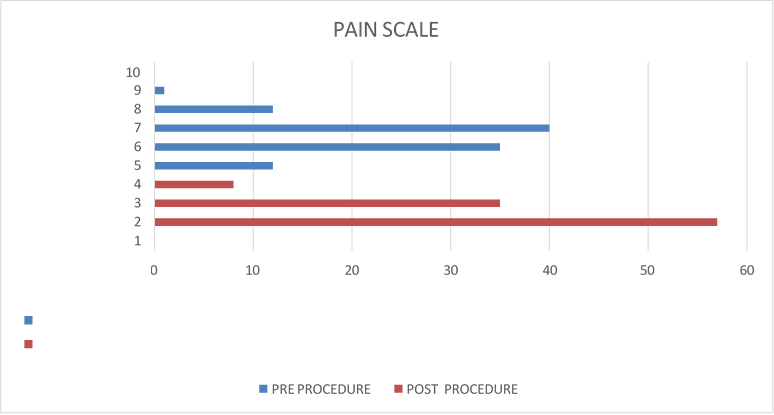
Figure 4
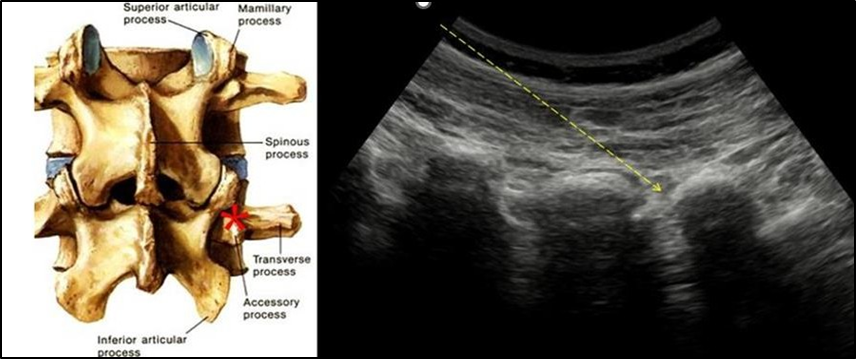
Figure 5
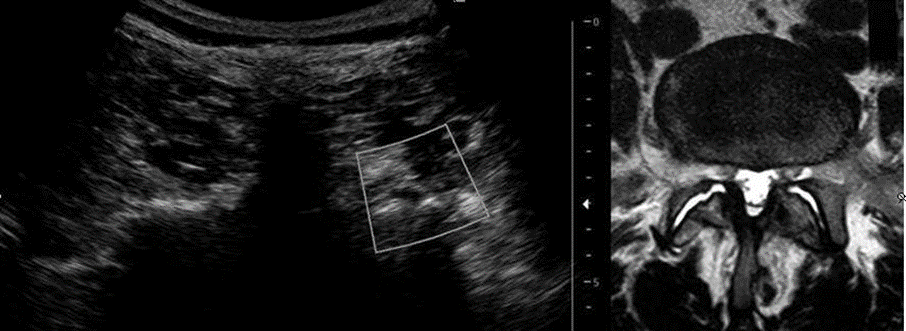
Figure 6
