Predisposing Factors and Maternal Outcomes of Ruptured Uterus among Pregnant Women at Bashair Teaching Hospital, 2022
Predisposing Factors and Maternal Outcomes of Ruptured Uterus among Pregnant Women at Bashair Teaching Hospital, 2022
Mahmoud Aljubeh1, Douha Abdalla2*, Mustafa Sabir Abakar Awad3 , Asma Mustafa Ahmed Ali4
1. Liverpool Women’s NHS Trust, Liverpool – United Kingdom.
2. Glangwili General Hospital, Carmarthen – Wales (UK).
3. Department of Community Medicine Al-Neelain University Faculty of Medicine, Khartoum – Sudan.
*Correspondence to: Douha Abdalla, Glangwili General Hospital, Carmarthen – Wales (UK).
Copyright
© 2024 Douha Abdalla. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 23 October 2024
Published: 01 November 2024
DOI: https://doi.org/10.5281/zenodo.14020853
Abstract
Background: Uterine rupture is an emergency and catastrophic obstetric complication associated with high maternal mortality and morbidity, especially in developing countries.
The incidence of perinatal mortality associated with uterine rupture is estimated to be around 11.2% worldwide. Others reported higher perinatal mortality rates, ranging from 25.5% - 85.4%, and maternal mortality rates, ranging from 3.3% - 9.8%.
The most common predisposing factor for uterine rupture is previous uterine surgery, and most cases involve women with a previous caesarean birth.
Objectives: To study the predisposing factors and maternal outcomes of rupture uteri among pregnant women attending Bashair Teaching Hospital, Khartoum, Sudan, from June 2021 to June 2022.
Methodology: This descriptive, cross-sectional hospital-based study was conducted at Bashair Teaching Hospital, Khartoum, Sudan, from June 2021–June 2022. The study involved 36 patients with uterine rupture. Data were collected via a predesigned, formal standardized (quantitative) questionnaire and analysed via SPSS 25.
Results: A total of 36 pregnant women with uterine rupture were included in this study. The mean age was 33± 9 years. More than half of them (55%) were aged 36-- 45 years, and the most common predisposing factor was previous caesarean section (47%), followed by obstructed labour and the induction of labour (20.3%). The most common complication was bleeding (42.9%), followed by bladder injury (20.6%), pulmonary oedema (15.9%), bowel injury (12.7%), and wound infection (7.9%).
Conclusion: Caesarean birth constituted the majority of the cases. Induction of labour and obstructed labour represented a significant percentage of the leading predisposing factors of uterine rupture. Caesarean section rates are increasing, and uterine rupture is expected to rise in tandem. There is an urgent need for evidenced based and up to date antenatal care practice and skilled labour staff, which should be emphasized through healthcare education
Predisposing Factors and Maternal Outcomes of Ruptured Uterus among Pregnant Women at Bashair Teaching Hospital, 2022
Introduction
Uterine rupture is an emergency and catastrophic obstetric complication associated with high maternal mortality and morbidity, especially in developing countries.
Uterine rupture is also associated with a high incidence of perinatal mortality of 11.2% and morbidity worldwide [1–4]. Other studies reported higher perinatal mortality rates, ranging from 25.5% - 85.4%, and maternal mortality rates, ranging from 3.3% - 9.8% [5,6]. Rupture of the uterus from any cause is a very serious obstetric complication requiring immediate surgical intervention to prevent maternal and foetal death [3], of which hypovolemic shock is the major cause [6]. The most common predisposing factor for uterine rupture is previous uterine surgery, and most cases involve women with a previous caesarean delivery [1].
Not all uterine ruptures present with the typical clinical picture of abdominal pain, hypovolemia, vaginal bleeding and foetal compromise. Therefore, maintaining a high index of suspicion for uterine rupture in women presenting with some, or all, of these features, regardless of parity, is important. Prompt recognition of uterine rupture and expeditious recourse to laparotomy are critical in influencing perinatal and maternal morbidity [1].
In Sudan, uterine rupture was the fourth most common direct cause of maternal death, accounting for 2.9% of maternal deaths [7]. It also complicated obstructed labour as the fourth sequel, with a percentage of 2.9% [8]. Recently, during this year in Sudan, maternal and perinatal mortality rates from uterine rupture were reported to be 14.3% and 92.8%, respectively [9]. The objectives of this study were to determine the incidence, maternal complications and management modalities of uterine rupture in pregnant Sudanese women.
Complete uterine rupture is a rare peripartum complication that is often associated with catastrophic outcomes for both mothers and babies [10]. A scarred uterus, most commonly due to a previous caesarean birth, substantially increases the risk of uterine rupture [10,11]. Few previous studies have described maternal outcomes after CUR, most likely due to the rarity of the event. Most previous studies were based on registries that used international diagnostic codes that did not differentiate between complete and partial ruptures. Moreover, previous studies have focused on outcomes, mainly in scarred uteri; few have described outcomes in unscarred uteri. Several, but not all, studies have reported that, compared with scarred uteri, ruptures are associated with worse maternal outcomes, such as hysterectomy, severe postpartum hemorrhage, and maternal morbidity, in unscarred uteri [12–14]. Regarding the maternal outcome. All medical records were reviewed for diagnostic accuracy. In Norway, all mothers with one previous caesarean delivery are offered trial labour unless there is an absolute contraindication against vaginal delivery [15]. Among women with previous caesarean sections, 64% underwent trial labour, and among these, 80% underwent vaginal delivery [16,17]. We aimed to identify maternal outcomes and their associated predisposing factors after CUR. Ruptures in unscarred uteri carry more catastrophic maternal outcomes, including hysterectomy, because they occur increasingly outside the lower uterine segment and extend more beyond the cervix.
This may indicate a delay in diagnosis due to a lower index of suspicion [18]. The incidence of uterine rupture among Sudanese women was 11:10,000. Most of the patients [81.8%] were less than 35 years of age. Most patients are managed by uterine repair, and severe hemorrhage is the most common complication [19].
As evident uterine rupture represents a major cause of maternal and foetal morbidity and mortality, and examining the predisposing factors that cause this issue can contribute to decreasing devastating outcomes and reducing the incidence rate.
The study aims to investigate the predisposing factors and maternal outcomes of rupture uterus among pregnant women attending Bashair Teaching Hospital, Khartoum, Sudan, from June 2021 to June 2022. We hope that the results of this study will help health care providers pay more attention to patients at risk for uterine rupture and treat and prevent complications associated with uterine rupture.
Methodology
Study design/setting
This was a descriptive, cross-sectional hospital-based study. It was conducted at Bashair Teaching Hospital, Khartoum, Sudan. It’s a tertiary setting hospital providing emergency room services as well as outpatient clinics in different medical proficiencies including Obstetrics and Gynaecology. The hospital is well staffed with obstetricians and gynaecologists, registrars, house officers, paediatricians, trained nurses, trained midwives and other supporting staff. There are 24-hour services with laboratories, blood banks and pharmacies. Additionally, an intensive care unit (ICU) and an isolated ward for antenatal and postnatal cases. The study took place between June 2021 -June 2022
Study population:
Pregnant women attending Bashair Teaching Hospital for delivery who developed rupture uteri during the study period.
Sample size:
A convenience sampling method was used to determine the sample size, whereas all pregnant women with rupture uterus either on attendance to the hospital or during active labour during the study period (one year) were included in the study. A total of 36 women were included.
Sampling method and technique:
Total coverage of all pregnant women attending for delivery at Bashair Teaching Hospital who developed rupture uteri.
Data collection:
The data were collected via a predesigned, formal standardized [quantitative] questionnaire. It was collected by the researchers, hospital registrars and well-trained house officers. The questionnaire included demographic data, questions to identify the predisposing factors for uterus rupture, and questions to determine the maternal outcome of uterus rupture.
Data analysis:
The data were analysed via the Statistical Package for Social Science [SPPS] version 25, and the results are presented in tables and graphs. The test of significance was calculated by the P value [0.05: 95% confidence interval].
Results
Sociodemographic characteristics:
A total of 36 pregnant women with uterine rupture were included in this study, and the mean age was 33 ± 9 years. More than half of them [55%] were aged 36–45 years, nearly two-thirds of the pregnant women [61%] resided in rural areas, only 22% were university graduates, and the majority [80%] were housewives, as shown in Table [1].
Table 1: Sociodemographic characteristics of the study subjects
|
|
N |
Percent |
|
|
Age groups |
15-25 years |
9 |
25.0% |
|
26-35 years |
7 |
19.4% |
|
|
36-45 years |
20 |
55.6% |
|
|
Total |
36 |
100.0% |
|
|
Residence |
Rural |
22 |
61.1% |
|
Urban |
14 |
38.9% |
|
|
Total |
36 |
100.0% |
|
|
Education |
Illiterate |
10 |
27.8% |
|
Khalwa (Traditional learning) |
10 |
27.8% |
|
|
Primary education |
8 |
22.2% |
|
|
University graduate |
8 |
22.2% |
|
|
Total |
36 |
100.0% |
|
|
Occupation |
Housewife |
29 |
80.6% |
|
Labour |
7 |
19.4% |
|
|
Employee |
0 |
0.0% |
|
|
Professional |
0 |
0.0% |
|
|
Total |
36 |
100.0% |
|
Nearly half of the patients [47.2%] were multiparous, 10 [27.8%] were primigravida’s, and 9 [25%] were grand multiparous women, as shown in Table 2.
Table 2: Shows the parity of the study patients.
|
Parity |
N |
Percent |
|
Primigravida |
10 |
27.8% |
|
Multipara |
17 |
47.2% |
|
Grand multipara |
9 |
25.0% |
|
Total |
36 |
100.0% |
All the patients presented either at term or as postdate pregnancies; more than two- thirds presented between 37–40 weeks of gestation, and the remaining presented more than 40 weeks of gestation [up to 42 weeks], as shown in Table [3].
Table 3: Gestational age of the study patients.
|
Gestational age |
N |
Percent |
|
37-40 weeks |
26 |
72.2% |
|
More than 40 weeks |
10 |
27.8% |
|
Total |
36 |
100.0% |
Predisposing factors:
The most common predisposing factor was previous caesarean section [47%], followed by obstructed labour and induction of labour [20.3%], previous uterine surgery [17.4%], a baby weighing more than 3.9, and multiple pregnancies [5.8%], as shown in Table [4].
Table 4: Shows the distribution of predisposing factors present among the patients.
|
|
Responses |
Percent of Cases |
||
|
N |
Percent |
|||
|
Predisposing factors |
Previous C/S |
17 |
24.6% |
47.2% |
|
Obstructed labour |
14 |
20.3% |
38.9% |
|
|
Induction of labour |
14 |
20.3% |
38.9% |
|
|
Previous uterine surgery |
12 |
17.4% |
33.3% |
|
|
Baby weight more than 3.9 |
8 |
11.6% |
22.2% |
|
|
Multiple pregnancy |
4 |
5.8% |
11.1% |
|
|
Total number of predisposing factors |
69 |
100.0% |
191.7% |
|
Complications:
The most common complication was bleeding [42.9%], followed by bladder injury [20.6%], pulmonary oedema [15.9%], bowel injury [12.7%], and wound infection [7.9%], as shown in Table [5].
Table 5: Complications of uterine rupture among patients.
|
|
Responses |
Percent of Cases |
||
|
N |
Percent |
|||
|
Complications |
Bleeding |
27 |
42.9% |
79.4% |
|
Bladder injury |
13 |
20.6% |
38.2% |
|
|
Pulmonary edema |
10 |
15.9% |
29.4% |
|
|
Bowel injury |
8 |
12.7% |
23.5% |
|
|
Wound infection |
5 |
7.9% |
14.7% |
|
|
Total number of complications |
63 |
100.0% |
185.3% |
|
Approximately two-thirds of the patients [66.7%] required blood transfusion for resuscitation of hemodynamic instability, as shown in Table [6].
Table 6: Percentages of patients who required blood transfusions.
|
Blood transfusion |
Frequency |
Percent |
|
Yes |
24 |
66.7 |
|
No |
12 |
33.3 |
|
Total |
36 |
100.0 |
Outcome:
Maternal mortality reached 33.7% of all patients who experienced uterine rupture, as shown in Figure [1].
Figure 1: Percentage distribution of maternal outcomes.
Pulmonary oedema was the sole predictor of maternal mortality, as 90% of patients with pulmonary oedema died. As shown in Figure [2].
Figure 2: Percentage distributions of complications across maternal outcomes.
There was a positive significant correlation between maternal age and outcome, as half of the patients aged 35--45 years died, whereas 0% of those aged 15--25 years died [P= 0.001]. Table [7]
Table 7: crosstabulation between age group and maternal outcome.
|
|
Outcome |
P value |
||||
|
Alive |
Died |
|||||
|
N |
% |
N |
% |
0.001 |
||
|
Age groups |
15-25 years |
9 |
100.0% |
0 |
0.0% |
|
|
26-35 years |
5 |
71.4% |
2 |
28.6% |
||
|
36-45 years |
10 |
50.0% |
10 |
50.0% |
||
Discussion
Uterine rupture is recognized as a life-threatening obstetric emergency, particularly prevalent in low-resource settings like Sudan. The findings of this study reaffirm the critical need to address the underlying risk factors contributing to this condition to improve maternal and foetal health outcomes.
The study revealed that the most significant predisposing factor for uterine rupture was a previous caesarean section (47.2%), consistent with other studies that highlight the vulnerability of scarred uteri to rupture during labour. This finding is in line with the study from Zhou et al. (2021) which reported a high incidence of uterine rupture associated with prior caesarean sections in China, emphasizing that the presence of a uterine scar considerably increases the risk of rupture during labour [20]. This trend is similarly observed in Western settings, where a history of caesarean section is a recognized risk factor for uterine rupture, as noted by Al-Zirqi et al. (2010) in Norway, where a previous caesarean section was also identified as a major risk factor for uterine rupture [21]. The increasing rate of caesarean deliveries globally raises concerns about a concomitant rise in the incidence of uterine ruptures. It underscores the need for careful patient selection and monitoring when opting for trial labour after a previous caesarean section.
Obstructed labour (20.3%) was the second most common predisposing factor, followed closely by induction of labour. The high rate of obstructed labour in this study highlights ongoing challenges in accessing timely and adequate obstetric care in Sudan, where delayed referrals and a lack of skilled birth attendants often complicate labour management. Igwegbe et al. (2013) reported similar findings in Nigeria, where obstructed labour was a major cause of uterine rupture due to prolonged labour and inadequate intrapartum care [22].
Maternal age was another significant factor influencing outcomes, with older women (36-45 years) experiencing higher mortality rates. This aligns with studies suggesting that maternal age is a risk factor for adverse obstetric outcomes, including uterine rupture. In contrast to a study by Al-Zirqi et al. (2010) in Norway showed significantly lower maternal mortality rates following uterine rupture, attributed to better healthcare systems, timely interventions, and availability of emergency obstetric services [21]. This stark difference underscores the impact of healthcare quality on outcomes. In well-resourced settings, maternal outcomes following uterine rupture are generally better due to more accessible advanced medical interventions.
Moreover, the study findings on maternal age and the risk of uterine rupture are consistent with results from You et al. (2018), who found that women aged over 35 years face higher risks for uterine rupture [23]. Advanced maternal age is often associated with increased parity and previous uterine surgeries, compounding the risk. In this study, multiparous women constituted 47.2% of the cases, further supporting the association between parity and uterine rupture risks.
The complications observed—bleeding, bladder injury, pulmonary oedema, bowel injury, and wound infection—reflect the devastating sequelae of uterine rupture. Hemorrhage was the most prevalent complication (42.9%), necessitating blood transfusions in 66.7% of the cases. The high rate of hemorrhage-associated complications highlights the critical need for efficient blood bank services and the availability of surgical expertise in obstetric emergencies. Pulmonary oedema emerged as a particularly lethal complication, with a 90% mortality rate among affected women, emphasizing the urgency of prompt recognition and treatment of such cases.
Overall, the maternal mortality rate in this study was 33.3%, which is substantially higher than the global average for uterine rupture. This alarming rate is indicative of gaps in the healthcare system, including delayed diagnosis, inadequate antenatal care, and limited access to emergency obstetric services. Comprehensive health education, timely diagnosis, and appropriate interventions are essential to prevent maternal deaths associated with uterine rupture.
Conclusion
Uterine rupture constitutes a major obstetric emergency in the study hospital and has potentially catastrophic implications for the mother and the baby. It is associated with high maternal and foetal mortality and morbidity. Previous C/S constituted the majority of the cases. The study’s findings underscore the importance of promoting antenatal care to identify high-risk pregnancies, particularly in women with a history of caesarean sections or complicated labour. Health education campaigns that emphasize the dangers of delayed labour management and the benefits of skilled birth attendance could help reduce the incidence of uterine rupture.
Recommendations:
The majority of uterine ruptures are avoidable. Strategies should be developed to improve access to healthcare services and to provide resources for dealing with obstetric emergencies. Females with previous C/S who are labouring should be closely monitored. Timely diagnosis and the implementation of prompt and appropriate interventions would aid in the survival of mothers and their babies. Induction of labour seems to be one of the leading causes of uterine rupture; thus, uterotonics should be used with caution, especially during augmentation in poorly progressing multiparous women and those who have had a previous caesarean section.
Declarations
Ethics approval and consent to participate:
The research ethical approval was obtained from the administration of Bashair Teaching Hospital.
An informed written consent was obtained from the study participants.
All ethical considerations were in accordance with the declaration of Helsinki.
Consent for publication: Not Applicable.
Availability of data and materials:
All data generated or analysed during this study are included in this published article.
Competing interests:
The authors declare that they have no competing interests.
Funding: Not applicable.
Acknowledgements: Not applicable.
Authors Contribution:
Mahmoud and Douha both have constructed the research idea, Mustafa collected the data and provided the formal analysis of the data, all authors contributed equally in terms of manuscript writing, data analysis and final manuscript preparation and editing.
References
1. Colin A. Walsh, MB, MRCPI,* and Laxmi V. Baxi M. Rupture of the Primigravid Uterus: A Review of the Literature. 2007.
2. Fenton PM, Whitty CJM, Reynolds F. Caesarean section in Malawi : prospective study of early. BMJ Br Med J. 2003;327[September].
3. McGrath J. Uterine rupture. Ir J Med Sci. 1962;38[1]:48–52.
4. Rouzi AA, Hawaswi AA, Aboalazm M, Fathia Hassanain, Sindi O. Uterine rupture incidence, risk factors, and outcome.
5. Peretz A, Grünstein S. Rupture of the gravid uterus. Gynecol Obstet Invest. 1962;154[5]:287–95.
6. Ekpo, E. E. (2000). Uterine rupture as seen in the University of Calabar Teaching Hospital, Nigeria: a five-year review. Journal of Obstetrics and Gynaecology, 20(2), 154–156. https://doi.org/10.1080/014436100629227.
7. Dafallah SE, El-Agib FH, Bushra GO. Maternal mortality in a teaching hospital in Sudan. Saudi Med J. 2003;24:369–72.
8. Dafallah SE, Ambago J, Faroug El-Agib. Obstructed labour in a teaching hospital in Sudan [Internet]. 2003. Available from: https://smj.org.sa/content/smj/24/1/37.full.pdf
9. Ali AA, Adam I. Maternal and perinatal outcomes of uterine rupture in the Kassala Hospital, east Sudan: 2006-2009. J Obstet Gynaecol [Lahore] [Internet]. 2011 Jan 31;31[1]:48–9. Available from: http://www.tandfonline.com/doi/full/10.3109/01443615.2010.522268
10. Ofir K, Sheiner E, Levy A, Katz M, Mazor M. Uterine rupture: Risk factors and pregnancy outcome. Am J Obstet Gynecol. 2003;189[4]:1042–6.
11. Smith JG, Mertz HL, Merrill DC. Identifying Risk Factors for Uterine Rupture. Clin Perinatol [Internet]. 2008 Mar;35[1]:85–99. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0095510807000899
12. Barger MK, Nannini A, DeJoy S, Wisner K, Markenson G. Maternal and newborn outcomes following uterine rupture among women without versus those with a prior cesarean. J Matern Neonatal Med [Internet]. 2013 Jan 25;26[2]:183–7. Available from: http://www.tandfonline.com/doi/full/10.3109/14767058.2012.725790
13. Zwart JJ, Richters JM, Öry F, De Vries JIP, Bloemenkamp KWM, Van Roosmalen J. Uterine rupture in the Netherlands: A nationwide population-based cohort study. BJOG An Int J Obstet Gynaecol. 2009;116[8]:1069–80.
14. Gibbins KJ, Weber T, Holmgren CM, Porter TF, Varner MW, Manuck TA. Maternal and foetal morbidity associated with uterine rupture of the unscarred uterus. Am J Obstet Gynecol [Internet]. 2015 Sep;213[3]:382.e1-382.e6. Available from:
https://linkinghub.elsevier.com/retrieve/pii/S0002937815005256
15. Al-Zirqi I, Daltveit AK, Vangen S. Infant outcome after complete uterine rupture. Am J Obstet Gynecol [Internet]. 2018 Jul;219[1]:109.e1-109.e8. Available from:
https://linkinghub.elsevier.com/retrieve/pii/S0002937818302916
16. DAVID A. MILLER, MD, T. MURPHY GOODWIN, MD, ROBERT B.
GHERMAN M, AND RICHARD H. PAUL M. Intrapartum Rupture of the Unscarred Uterus. Elsevier Science Inc; 1997.
17. Al-Zirqi I, Stray-Pedersen B, Forsén L, Vangen S. Uterine rupture after previous caesarean section. BJOG An Int J Obstet Gynaecol. 2010;117[7]:809–20.
18. Al-Zirqi2019.Pdf.
19. Ahmed MA, Elhassan G, Elkhatim S, Mohamed EY, Ribat TN, Medicine CC. Rupture Uterus in Sudanese Women : Management and Maternal Complications [Internet]. Vol. 4, World Journal of Pharmacy and Pharmaceutical Sciiences. 2015. p. 1669–75. Available from: www.wjpps.com
20. Zhou, Y., Mu, Y., Chen, P., Xie, Y., Zhu, J., & Liang, J. (2021). The incidence, risk factors, and outcomes of uterine rupture during different birth policy periods: an observational study in China. BMC Pregnancy and Childbirth, 21(1).
21. Al-Zirqi, I., Stray-Pedersen, B., Forsén, L., & Vangen, S. (2010). Uterine rupture after previous caesarean section. BJOG: An International Journal of Obstetrics & Gynaecology, 117(7), 809-820.
22. Igwegbe, A. O., Udegbunam, O. I., & Eleje, G. U. (2013). Risk factors and perinatal outcome of uterine rupture in a low-resource setting. Nigerian Medical Journal, 54(6), 415-419.
23. You, S. H., Chang, Y. L., & Yen, C. F. (2018). Rupture of the scarred and unscarred gravid uterus: Outcomes and risk factors analysis. Taiwan Journal of Obstetrics and Gynecology, 57(2), 248-254.
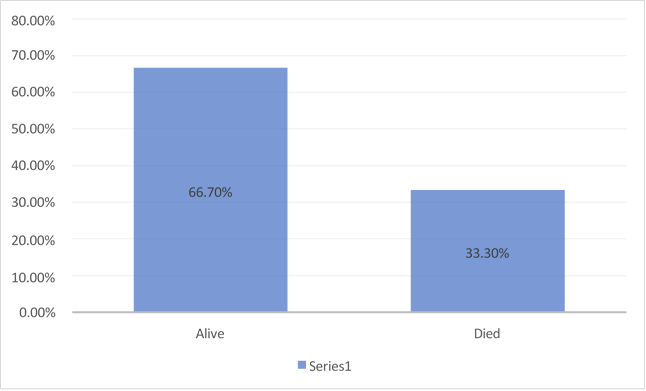
Figure 1
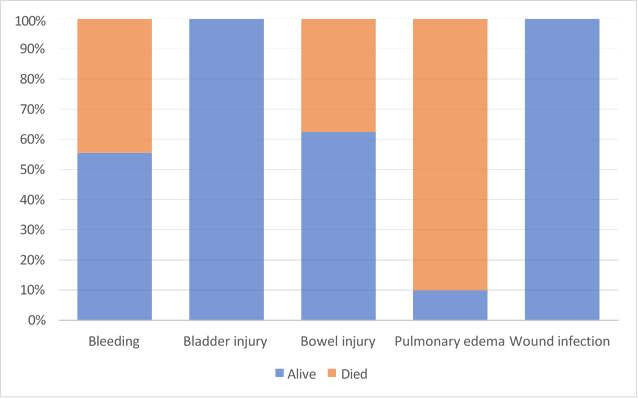
Figure 2
